By Lewis Lennard
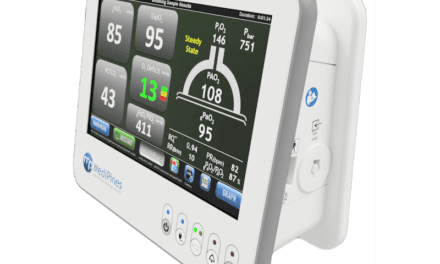
Patient monitors continuously observe vital signs—which communicate a patient’s condition and disease severity to clinicians—and provide warnings in the case of a serious event. Any anomalous vital sign values should alert clinicians and, to some extent, provide direct physiological input data to control connected life-support devices.
COVID-19 and other factors have led to a surge in patient admissions, increasing the demand for patient monitors worldwide. Moreover, aging populations, the increasing complexity of patient conditions, and healthcare cutbacks have taken their toll on healthcare organizations. Plus, a shortage of clinicians—along with technological advancements—has led to the proliferation of remote patient monitoring.
Users Beware
Vital signs monitors frequently top the U.S. FDA’s recall list, due to their ability to cause patient harm. In fact, the FDA database includes many reports of non-invasive blood pressure (NIBP) failures, incorrect oxygen values, electrocardiogram (ECG) signal errors, and failure to sound alarms for anomalous vital sign values. This compounds the importance of ensuring patient monitoring systems are accurate and safe to use.
In short, patient monitors must provide accurate data across all available vital signs. Such accuracy is verified on a periodic basis, based on risk assessment, manufacturer recommendations, and stages of the monitor’s lifecycle. Moreover, like all healthcare technologies, these monitors must be frequently checked and tested to ensure that they work accurately and aren’t harmful to operators or patients. That’s why regular performance tests are essential.
Performance tests are typically executed using calibrated simulators across several vital signs parameters and are all part of an acceptance test, a preventative maintenance cycle, or a repair. A typical test cycle for a vital signs monitor may include a visual inspection; self-tests; electrical safety testing; integrity of the device under test; parameter accuracy of temperature;, and pressure, SpO2, ECG, and respiration tests. Alarms checks for pitch, frequency, and volume are also required, along with dynamic physiological simulations.
Patient simulation is implemented according to the following performance verification procedures from medical device manufacturer service manuals. Ideally, a multi-parameter patient simulator is used to test a device in one sequence, which provides a practical approach for HTM professionals. Note: Each parameter has a different method for performance testing.
- Noninvasive blood pressure: NIBP measurement principles primarily rely on the oscillometric method, which determines systolic, diastolic, and mean arterial values by detecting the vibrations in the arterial wall at various pressure points via an inflated cuff. Moreover, testing the accuracy of the monitor involves both static and dynamic pressure simulations at specific values, with system leak and over-pressure tests also part of the procedure. To ensure patient safety, such tests are executed using a manometer and a built-in pump.
- Invasive blood pressure: IBP is an invasive form of blood pressure measurement and uses a liquid-filled catheter, which is placed in an artery. The arterial pressure is converted by a pressure transducer into an electrical signal—typically, 5µV/V/mmHg. Testing the monitor for its linear sensitivity is essential in determining its accuracy. Patient simulation is performed by outputting defined direct current volts, or DCV, values.
- Pulse oximetry: SpO2 estimates the amount of oxygen in the blood by analyzing the absorption of light by hemoglobin across two different wavelength light-emitting diodes (red/infrared). If more red than infrared light is being absorbed, there are less oxygenated blood cells. SpO2 simulation is often implemented using optical simulation “fingers.” These devices provide variable attenuation to light in the red and infrared wavelengths.
- Electrocardiograph: ECG measures tiny electrical signals from the heart using ECG leads placed on various parts of the body. These signals are amplified, measured, and displayed on a patient monitor. ECG simulations are electrically generated cardiac arrhythmias or performance waveforms with pre-set amplitudes and frequencies.
- Respiration: Respiration utilizes the ECG leads to measure transthoracic impedance. As the thoracic cavity expands during inspiration, the impedance of the chest increases; during expiration, the impedance of the chest decreases. Simulating respiration involves set baseline impedances, with delta impedances providing respiration rates.
- Temperature: Negative Temperature Coefficient thermistors typically measure the temperature of patient monitors. This means that when temperature increases, the resistance of the thermistor decreases. Temperature simulation is provided through a set number of resistances, depending on the type of sensor (YSI400/YSI700).
Time to Test
So, why is it important to test? In short, the proper operation of medical equipment is equally as important as the function it performs. And like all technologies, healthcare equipment must be thoroughly checked and regularly tested to ensure that it works effectively and doesn’t pose a risk to operators or patients.
After all, an incorrect reading or missed condition might have considerable consequences for the patient; therefore, the person maintaining the patient monitoring system must be technically competent, appropriately trained, and aware of the various parameters being verified. Although the equipment manufacturer is ultimately responsible for providing verification procedures to achieve optimum performance, the person or organization maintaining the device must understand the required procedures and operation of the equipment. Any doubt? Contact the manufacturer.
Planned preventative maintenance is another important aspect of managing electrical healthcare equipment, such as patient monitoring devices. To keep both the patient and operator safe, procedures are required to cover visual inspection, electrical safety testing (typically, NFPA 99), performance or functional testing, and record-keeping.
Always ensure that the function and operation of the device under test is understood before instituting planned preventative maintenance. Without fully understanding the function and/or operation, visual inspections, electrical safety tests, and functional tests might be incorrect or incomplete. Finally, before testing any patient monitoring system, ensure that the manufacturer’s recommendations are available since they often supersede any general inspection guidelines.
Real-World Evidence for Patient Monitor Testing
To sum it up, regular performance checks keep patient monitoring devices running properly, which is essential for patient care. It’s something Marta Villarejo, PhD, director of general biomedical device service at Hermed Spain, has seen firsthand.
She says the Spanish company utilizes Rigel Medical’s Uni-Sim vital signs simulator and the Rigel 288 Plus electrical safety analyzer—with the first tool particularly benefiting Hermed Spain. “By bringing together NIBP, SpO2, ECG, temperature, [invasive blood pressure monitoring], and respiratory functions in one piece of equipment, the Uni-Sim Vital Signs Simulator greatly facilitates the field service activities by Hermed engineers, saving time and avoiding the need to carry several pieces of equipment.”
In conclusion, with HTM professionals busier than ever, vital signs and patient monitoring test equipment will help them meet compliance and performance requirements. It will also allow them to maintain safety without imposing an overly excessive test regime.
Lewis Lennard is an application engineer at Rigel Medical. Questions and comments can be directed to 24×7 Magazine chief editor Keri Forsythe-Stephens at [email protected].