In today’s difficult fiscal times, everyone is searching for places to cut spending. Often-targeted sources of spending include the training and travel budget. Perhaps, instead of cutting training dollars, we should increase them. As the old adage goes, “You need to spend money to make money.” In the case of clinical engineering, perhaps we can change that to, “You need to spend money to save even more money.”
The task of managing a successful clinical engineering program has become significantly more difficult as budgets have tightened. Spending is being scrutinized. Vendors are increasing service costs for both “time and materials” and service contracts. Parts costs are increasing, and we are challenged to “do more with less.”
As I speak with my peers in the industry, I get a sense that service costs are being rolled into acquisition costs. Recent negotiations I have been involved in have shown that vendors are heavily marketing point-of-sale extended warranties and service contracts. It would be easy to purchase a 5-year service contract at the time of sale in an effort to show a reduced departmental budget. However, is this the right thing to do? I would argue that many times the answer is no.
As budgets decrease, perhaps clinical engineering should begin assessing cost of ownership instead of focusing solely on cost of acquisition. If we can show that standardizing inventory wherever clinically possible and bringing talent in-house, combined with creative maintenance strategies will result in a net savings, even the most budget-minded administrator will begin to see value in the clinical engineering department. As our real and perceived value increases, so too does our ability to obtain funding for necessary tools. One such tool is training.
What If They Quit?
There are many arguments presented stating why spending significant amounts of time and money training technicians is not a good idea. The thought that we risk losing employees once we have trained them represents one point of resistance repeatedly brought up. No one wants to be a training ground for our vendors or our competitors. One method of mitigating this issue is through the use of a contract with the employee. In simple terms, the employee is responsible for reimbursing the employer should he/she leave before an agreed-upon period of time. This agreement can be prorated.
While some managers may at times use training as a reward for employees that provide exceptional service, I personally disagree with this methodology. When determining training paths, look at the long-term goals of both the employee and the department. At each employee performance review, I ask every technician, “What area of specialization interests you?” This way, I can tailor training to the desires of the individual. Training your brightest tech in lab equipment to ensure he or she will begin to specialize in lab equipment is not going to bring job satisfaction to that employee if they prefer working in the operating room. The desires of individual staff members must of course be balanced with the needs of the department. We can’t have every technician work as a CT specialist.
It is also important to honestly evaluate skill sets. An employee with great networking skills and poor mechanical skills may not be the best choice for sterilizer training.
Finally, we must consider our compensation package. If the organization across town can offer $2 per hour more in salary, we risk losing our investment. It is important to stay competitive.
Eventually, however, we will lose employees. It is important to have a backup plan prior to lobbying for a training budget. Expect the administration to ask for this plan. Some contingencies to explore include:
- A strong cross-training program. Set aside time for formal cross-training. Do not rely on on-the-job training (OJT), although OJT is certainly an important component of training staff members.
- Develop a succession plan. As technicians mature and grow in their roles, it is essential to develop a succession plan from the top to the bottom of the department. In some cases, this plan will include bringing in talent from areas outside of the organization.
- Be active in the local biomedical/clinical engineering community. While “poaching” valuable employees from other organizations is never a good idea, a fact of life is that technicians want to expand their horizons. There is a difference between offering a technician a growth opportunity and poaching. Do not cross this line, as it may cause difficulty at a later date.
- Maintain a good relationship with equipment vendors. In the event of an unexpected gap in trained technicians for a given modality, it is possible to augment current skill sets with restructured service agreements. Ensure that language exists in these contracts with no penalty changes for this unforeseen event.
Calculating the Expense
The next obstacle in procuring training dollars is showing a return on investment (ROI). All too often as clinical engineers, we think in black and white, or in this case dollars spent compared to dollars saved. The obvious formula to determine ROI for training is to obtain a quote for a service contract and compare that to the cost of training plus specialized tools and test equipment. This may not be a true indication of our ROI. Instead, we need to consider other issues. For instance, if a piece of equipment covered by contract (or time and materials) has limited vendor support due to geographic limitations, how much in dollars does downtime cost? As an admittedly extreme example to show the concept, if a CT scanner is down and we cannot get vendor service on-site for 24 hours for a simple fix that requires no parts, how much revenue was lost? Not only do we lose revenue from CT studies, we risk losing other revenue—such as placing head trauma patients on divert in the emergency department.
The decreased ability to care for our patients is a consideration apart from revenue. I’ll save that discussion for another time. By carefully tracking service history for vendor-supported equipment, it is possible to start gathering this data and presenting it as part of our ROI.
Make Smart Choices
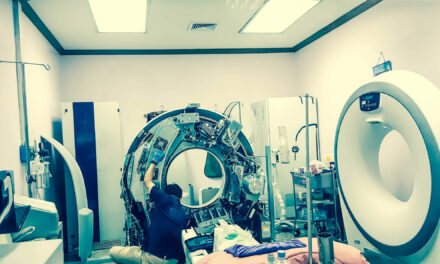
When determining where to spend a limited training budget, it is vital to choose wisely where the resources are spent. Do we send a staff member to training for an MRI unit, for instance?
At first glance, it may look like canceling that MRI contract and bringing service in-house will net a big savings. A closer examination may show that we do not have a great ROI. The savings for a single machine may not prove cost-effective, and the technical skill set may not develop quickly. If, however, there are multiple units, the ROI increases greatly, as does the technical skill set.

Even in today’s difficult fiscal times, spending money wisely, such as on training, can ultimately save even more money.
When considering providing training, we need to determine if the correct staffing is available. Items to consider here:
- How many new technician-hours will be required to support this device?
- Does your staff have the requisite skill sets to successfully complete training?
- Does your staff have the skill sets to provide proper support upon completion of training?
- What are typical service coverage hours for this equipment?
- How will you support this equipment during vacations or other absences?
Other considerations include:
- What specialized tools or test equipment are required?
- Are there additional space requirements?
- Are there other infrastructure requirements, such as a clean room or medical gases?
- Are there additional skill sets required, such as cryogen training?
Evaluate the total cost of support when calculating ROI for training.
We Can Do It
When proposing training for equipment currently maintained by vendor or third-party support, it is essential to gain the support of the end user. This may be a relatively simple or somewhat difficult task, depending on the relationship between clinical engineering and the end user. Clinical engineering typically has a long history with the operating room staff. This may pave the way to expanding service in that department. Less traditional areas such as CT, MR, or the lab require a bit more work.
One method of gaining the trust of departments for which a clinical engineering department has not historically provided extensive support is shared service agreements. The shared service model has some advantages when cultivating new service relationships.
The shared service agreement is typically significantly less expensive than a full service contract due to the reduced hours needed by the vendor to support the equipment covered by the contract. The end user maintains a level of comfort knowing that the vendor will always be available, should clinical engineering be unable to resolve a particular issue. I have gone as far as assuring an end user that the clinical engineering staff will contact the vendor for support if a resolution is not in place within a specified period of time, such as 3 hours.
With shared service, the department maintains a relationship with the vendor. I have often reassured vendors that by entering a shared service agreement, everyone wins. The facility lowers costs while reducing response time; the vendor keeps a contract in place, thus assuring continued justification for staffing; and clinical engineering gains experience, which enhances their reputation with the end user. The vendor service personnel will often provide further training in an OJT manner for in-house staff. This further enhances the knowledge and skill sets of clinical engineering staff. Show that you can and will do the job quickly and efficiently.
It is also possible to negotiate significant savings in tuition costs when discussing a cooperative service arrangement with a vendor.
Report Your Success
Convincing executive leadership to invest one time in training may be a fairly simple task. How do we convince them to continue investing in training? The simple answer: We show success. The difficult part is measuring and proving success.
As discussed earlier, ROI is the main method to show fiscal success. Do not get caught forgetting to report the intangibles, such as reduced downtime. It is very important to capture all service events. By capturing all service provided, you can compile an accurate picture of the value clinical engineering has provided.
Fiscal success is not the only payback for investing in our staff. Throughout the initial months of increased responsibility, check with the users and the managers to ensure satisfaction is high. Gather the support of department managers and directors. By involving these critical decision-makers, it becomes easier to show success and to continue expanding in-house offerings.
Sell, Sell, Sell!
All too often, clinical engineering leadership works on the approach of “fly under the radar.” If executive leadership does not hear about us or think about us, we cannot get in trouble. This can backfire when trying to negotiate a training budget. Worst-case scenario in my mind would be trying to build a training budget and receive the response, “Who are you, and why exactly are you asking me for $50,000 to train employees that should already know how to do their job?”
In my department, the phrase, “Perception is reality” is often heard. If we “sell” our department—meaning, we teach senior clinical staff and executive leadership that clinical engineering provides a valuable service, that we employ highly skilled professionals, and that we can provide excellent customer service and do so at a cost savings—then the conversation with executive leadership becomes more manageable. Instead of, “Who are you?” it becomes, “Tell me what I get for my $50,000.” It is then our job to sell.
Our selling points are:
- Return on investment.
- A rapid physical response to a downtime situation.
- Customer (both internal and external) satisfaction.
- Improved employee satisfaction and retention.
Don’t get caught in the “I can’t get no training budget” blues. Get out there and show the value that training brings to your organization.
Dan DeMaria, CBET, has worked in the profession for 29 years and is a biomedical engineering and telecommunications manager. For more information, contact .