How a chasm formed between clinical engineering departments and executive offices, and what steps we can can take to bridge it
?Last year, after 17 years in the biomedical equipment repair industry, I hung up my multimeter leads and headed off to grad school to pursue a dual master’s degree in healthcare administration and business administration. Immersing myself for a year in an accelerated MHA/MBA program allowed me to expand my view of healthcare to include its history, its disciplines, its laws, and everything related to the business side of how we deliver care to patients in America. My program was thorough, providing deep dives into every aspect of contemporary healthcare management. That’s why I was shocked to find little to no mention of my previous field, whether one calls it healthcare technology management (HTM), clinical engineering, biomedical engineering, clinical technology services, or simply medical maintenance. (For the purposes of this article, I will refer to these activities collectively as “clinical engineering.”)
Regardless of the department name, however, there is a common denominator that I believe many biomedical technicians would agree with: There is a huge chasm in most institutions between clinical engineering departments and the hospital C-Suite.
In the current healthcare environment, healthcare systems across the nation—both public and private—are trying to reduce their costs. Declining Medicare reimbursement rates and the recent recession have hurt hospitals in a major way. The healthcare industry is searching for ways to bend the cost curve, and some believe that the solution may be to leverage technology to create safer, more efficient healthcare solutions.
Despite this situation, healthcare organizations tend to undervalue the very group that should be able to quarterback the cost-effective, right-sized technological solutions for hospital needs: the clinical engineering department. This underutilization of clinical engineering, caused by the gulf that exists between the C-Suite and the clinical engineering departments that serve them, results from a lack of communication and understanding. It is the duty of clinical engineering to engage the healthcare system at all levels. In this article, after explaining the reasons for this disconnect, and suggesting what the ramifications are, I will propose a system of engagement with which departments can measure their own level of connectivity to the C-Suites that lead them.
The Rising Cost of Healthcare
Technological innovations have been cited as being the single most important factor contributing to the rising cost of medical inflation in the second half of the 20th century. These innovations have accounted for about one-half of the total rise in real healthcare spending over the past several decades.1
There are a few reasons for this. First, from a clinical or ethical standpoint, there is the technological imperative. Providers and even administrators feel it is their duty to provide the latest state-of-the-art items. However, once a technology has reached a mature state, the improvements or gains yielded by newer models are sometimes marginal at best.
There are also strategic reasons for innovation driving cost. It behooves a healthcare system to have the highest level of technology in place in order to differentiate our systems from our competitors. This results in a sort of “technological arms race,” pitting one healthcare system against others in their service market, while producing financial gains for the manufacturers and vendors standing by.
Physicians also play a role in this trend. We’ve all had the experience where physicians demand certain items. These physician preference items result when physicians have specific desires for equipment based on nonobjective reasons, such as past experience working with the equipment, a colleague’s recommendation, or even direct input or sales influence from the vendor representative.
Another factor driving the cost of healthcare from an innovation standpoint relates to a lack of planning on behalf of the healthcare organization. How many times have we seen devices or systems prematurely replaced or abandoned because they do not meet facility, plant, or IT-interoperability requirements? A lack of coordination during the procurement process can have devastating results and create massive amounts of lost value for the system.
In each of these cases, clinical engineering departments have the distinct ability to mitigate these risks. An engaged clinical engineering department that effectively manages a life-cycle management process and employs technology assessments of all potential equipment purchases will be able to ensure that only items that offer the most needed value to the organization are purchased. A thorough check from other clinical engineering peers and organizations such as the ECRI Institute will lend valuable, data-driven decision-making as to which product offers the most potential to serve the hospital’s end users.
In an environment of increasingly scarce funds for capital equipment, objective reasons should be used when determining technology purchases. Clinical engineering not only possesses the resources to facilitate this, but these departments are also plugged into nursing, medicine, facilities management, and IT—all the stakeholders who need to be communicating to implement a comprehensive capital equipment replacement plan.
So if this is the case, why is it such a challenge for clinical engineering to be invited to the table to participate in these conversations?
Causes of the Disconnect
There are many reasons for the current disconnect that exists between many healthcare C-Suites and their respective clinical engineering departments. They fall under four categories.
The Technological Divide. Although clinical engineering departments play a vital role every day in our healthcare facilities, many people do not know exactly what all we do. Ask the average person outside of the hospital walls what a clinical engineer or biomedical equipment support specialist does, and you’ll get a blank stare. Even within our hospital walls, there are many healthcare professionals who do not fully grasp the entire scope of what services clinical engineering departments offer the organization.
Another factor in the technological divide relates to the aim of the biomedical equipment support specialist: to never have to be called. Most of us define success as the systems we support not failing. Biomedical technicians specialize in being proactive and operating around the clinicians and technologists so that there is a seamless delivery of healthcare to the patients. Equipment receives preventive maintenance early in the morning, late at night, or on days when the clinic isn’t scheduled to see patients. If a device does experience some sort of malfunction, biomedical technicians bend over backward to make sure that it is immediately rectified, by any means possible. If a technician—or, more broadly, a clinical engineering department—is doing its job, rarely will issues be elevated above the level of the end user or department head.
This creates a bit of a conundrum for biomedical departments who want to be on the C-Suite’s radar and have a seat at the table. Clinical engineering departments strive to be invisible when it comes to the delivery of care, but without processes or structures in place for the clinical engineering department to have an audience with the C-Suite, clinical engineering departments may be forgotten when it comes time to make facility decisions related to equipment purchases, renovations, rollouts, patient safety investigations, or system redesigns.
Administrator Education. What are healthcare administrators learning about clinical engineering in school? As noted, I have been surprised at the almost total lack of attention paid to the field. Students pursuing their Masters in Healthcare Administration or other healthcare degrees will pore over pages learning about healthcare delivery systems, finance, economics, project management, operations, quality, and even healthcare technology and IT. But rarely do textbooks or journals discuss the role of those who manage medical equipment.
This means that healthcare executives and other leaders in the industry who graduate from these programs are essentially transitioning from the academic environment to the hospital environment without an understanding of what clinical engineering is or what biomedical equipment support specialists do. Until they have personal, firsthand experience talking or working with a biomedical professional, a gap will exist in their ability to make use of all available resources in day-to-day decision-making. During my graduate studies, I found no mention of clinical engineering, capital equipment replacement strategies, or the benefits of what a clinical engineering department can do for the organization.
I don’t believe that my program is unique in this regard, as numerous literature reviews on the subject have yielded nothing. I was shocked by this. I did find one instance of a reference to “biomedical devices” in a book about healthcare IT, but again and again as I surveyed the literature, there was no mention of the HTM field. The reason for this, I believe, is what I call “the publishing problem.”
The Publishing Problem. When I tackled the issue of searching for articles that illustrated how clinical engineering departments could lend themselves to cost savings at healthcare facilities, I had a difficult time finding any articles in healthcare management journals or magazines. However, I had no trouble finding them in journals that clinical engineers and other biomedical equipment professionals read. There is no shortage of articles that argue how important clinical engineering departments are, how vital this profession is, and how hospitals need to utilize them to achieve their bottom line. The only problem is that these articles only tend to appear in publications such as the Journal for Clinical Engineering, Biomedical Instrumentation & Technology, IEEE, and 24×7. However, healthcare administrators generally do not read these publications. Rather, they read the Journal for Healthcare Management, the Journal of Healthcare Finance, Health Affairs, and Healthcare Executive.
Essentially, clinical engineers, who tend to be the most prominent publishers in our field (in academic texts), are preaching to the choir, celebrating the importance of the clinical engineering field—to other clinical engineers. This lack of cross-pollination between clinical engineers and healthcare administrators does nothing to close the gap of understanding between these two professions. The only exception to this that I found in a thorough lit review was an article in Healthcare Finance back in 1995 by David Dickey.2 However, one article published in the past 20 years is simply not enough to raise awareness of the cost-saving potential of engaging clinical engineering departments.
This lack of publishing has longer, more far-reaching implications. Textbooks are written based on literature reviews. Most everything that appears in the pages of a textbook in an MHA program is cited with references. I am not surprised that there was a dearth of information about the role of clinical engineering departments in my texts. The people who wrote or assembled the textbooks probably never saw anything articulating the value of clinical engineering in their research.
Humility Versus Self-Promotion. Anyone who has worked in clinical engineering or around clinical engineering knows that people who gravitate toward this field tend to possess a certain range of qualities. The biomedical technicians I have worked with tend to be intelligent, funny, sarcastic, dedicated, loyal, and sometimes more than a bit rebellious. However, another common characteristic is humility. Biomedical professionals are not often drawn toward mechanisms that may help market ourselves, our accomplishments, or our value. These mechanisms usually don’t exist on their own within healthcare organizations unless we create them.
As mentioned before, minimizing downtime is the goal, and crisis equals failure. For a successful biomedical department, a crisis may be the only time they end up having a seat with the executive leadership—and nobody wants to be meeting under those conditions. We have that behind-the-scenes standard of success: “No news is good news.” The colleagues who I have worked with over the past 20 years have usually been happy to be in the shop, out of the limelight, and working on equipment. However, without biomedical professionals taking a proactive stance on communicating value, healthcare leaders may fail to fully recognize the full breadth of what biomedical departments can accomplish.
A Call to Action
Do you know the names of everyone in your C-Suite or executive leadership team? Are you familiar with the goals and objectives of your C-Suite? Do you know what most concerns your chief financial officer? What are your hospital’s capital priorities this fiscal year? When was the last time you sat down with the chief information officer, or the IT staff (when there wasn’t a problem)?
Clinical engineering departments need to ensure that they are taking proactive steps to engage the C-Suite if they hope to be fully utilized. How does your facility view your clinical engineering department? Do they view you as simply a “break-fix” service? If so, you are a service that is ripe for outsourcing. If your organization doesn’t know where you are located, if they don’t realize what level of sophistication you can support, if they don’t think you are financially savvy, if they don’t believe you know how to communicate, or if they don’t have any idea what it is that you do, you are failing not only your organization but also your own department.
Strategies to Engage the C-Suite
So what can biomedical professionals and clinical engineering departments do to combat this?
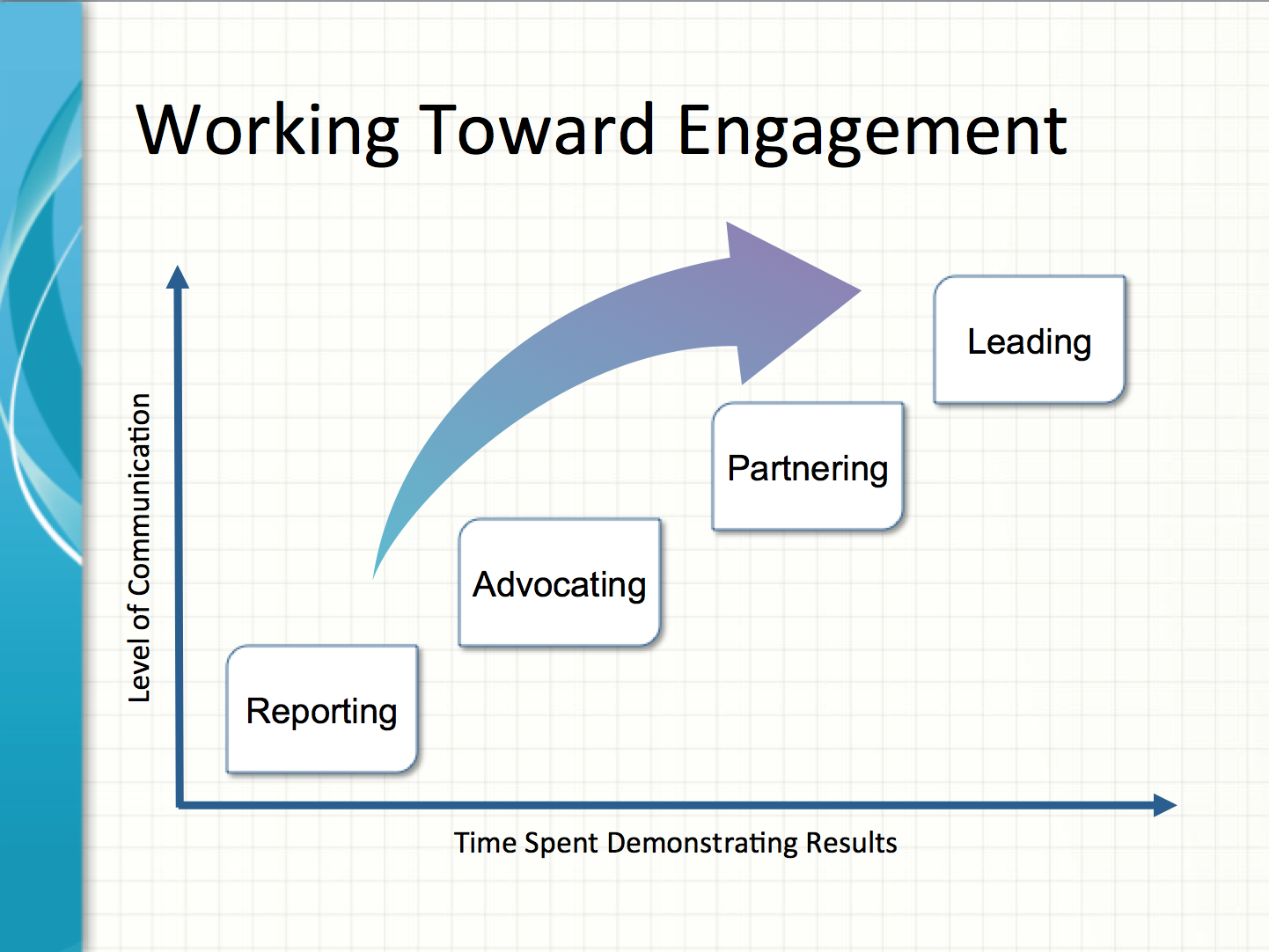
In working toward greater engagement with the C-Suite, I propose that clinical engineering departments can achieve four levels of engagement with their healthcare organization: Reporting, Advocating, Partnering, and Leading.
As you can see in the accompanying figure, the x-axis represents time spent demonstrating results, while the y-axis represents the level of communication or effort expended communicating value. The figure attempts to convey the message that it doesn’t matter how strongly you advocate for your department if you are not achieving substantial results. Likewise, your department’s value will be diminished if you are achieving results but the hospital doesn’t know about all that you are doing for the organization.
Reporting. My belief is that departments that merely maintain equipment (preventive maintenance, calibration, repair) and report compliance for Joint Commission standards are operating at the most basic level of engagement with their organization.
Even if your department is in the reporting phase of engagement, re-examine how you report information upward. How and what you report upward can affect your presence in the facility. Healthcare executives need data that is meaningful, timely, and succinct, and that aligns with goals and objectives.
Often, visual data representations, such as dashboards, work best. Synthesize your data down to key performance indicators that quickly let them know how your department is doing and clearly call attention to areas that may require additional support. Avoid using too much jargon, and ensure that you clarify and explain data. Always use professional terminology when referring to your department and your people and their roles.
Go beyond the standard metrics of PM completion, number of devices serviced, and downtime totals. Illustrate your department’s cost savings to include benchmarking against other sites in your system if you have access to the data. When in doubt on what to report, speak to the bottom line, whether that is illustrating cost-avoidance, showing how a contract that was brought in-house saved money, or highlighting a way that a technological solution can achieve big savings for the system.
From a soft-cost standpoint, demonstrate how safety is enhanced via the number of health device hazards you have completed and the number of manufacturer recalls you have responded to. Additionally, if you use customer satisfaction surveys, make sure you communicate these results upward. This is information that your leadership will want to know, and that may either validate you as a service or show that you need more resources.
Advocating. Departments that advocate are the ones that are attempting to reach out to their organization to push for cost-saving measures or to help the hospital do the right thing. This may take the form of trying to elevate awareness of a piece of equipment that needs replacement, asking for additional resources, highlighting a patient safety issue, or recommending going with one system over another at the time of procurement. I believe the majority of biomedical departments are operating at this level of engagement—reaching out to their organization but perhaps lacking a systematic methodology for doing so.
If you are operating at the advocating level, remember a key point: Advocating is different from whining. When trying to convince the organization of what clinical engineering feels is the best move, tell your story. Provide context, and make it relevant. Ensure that those higher up in the food chain are aware of your situational reality and the challenges that you may face. Demonstrate how the actions or resources that you are lobbying for will save the hospital money in the long run or enhance patient safety. Always illustrate the return on investment of these recommendations, as evidenced by cost-benefit analyses. Be persistent yet tactful.
Partnering. The next level of engagement—Partnering—in this context means that clinical engineering department managers or representatives have a seat at the table when the healthcare organization is making key decisions. If the facility is looking to make capital equipment purchases, deliberating on how to best renovate an existing space, deciding on a healthcare technology platform, or investigating a near miss, a representative from clinical engineering will be in the room and weighing in on the conversation. If an organization routinely says, “We should not proceed without having clinical engineering in the room,” then that clinical engineering department has achieved the Partnering phase.
You need to ensure that your organization allows you a seat at the table when appropriate. Assess your department’s presence in the organization. What committees are you on? Does the C-Suite know to check in with you before making a move? How often do you need to clean up a mess because your department wasn’t involved from the get-go? In this current healthcare environment, no organization can afford to have equipment languishing in the warehouse because of a failure to properly coordinate purchase, assembly, installation, or IT integration. Make sure that you are on everyone’s radar, and that your department has an equal say in planning, technology assessments, service and support contract decision-making, and orchestrating hospital projects.
Leading. If you are achieving all of the previously mentioned strategies, consistently and with results, it is to be hoped your organization will come to understand the full value of the clinical engineering department and invite you to take a leading role. This may lead to clinical engineering departments driving change rather than simply facilitating it, heading IT departments and initiatives, formulating organizational strategy, and perhaps even one day operating at the C-Suite level.
Imagine a healthcare organization where the head of clinical engineering is a vice president, or reports directly to the CEO. Perhaps the chief technology officer is a clinical engineer or other degreed professional who has a biomedical equipment background. Perhaps this biomedical CTO also oversees the IT department! A facility that allows clinical engineering to guide them during key decision-making events, whose strategic planning is informed by or even led by clinical engineering, whose overall operational efficiency and Lean methodology is informed and empowered by the power of leveraging healthcare technology, has allowed their clinical engineering department to have a leading presence.
Missed Opportunities
Anyone who has worked in clinical engineering and felt like their department didn’t have a big enough presence in their facility has probably seen some of the same mistakes repeated. How many times have you grumbled because a device or system was replaced prematurely? You may have seen misguided or even incomplete purchases. Maybe you’ve seen installations or projects stall out because of a failure to properly coordinate the needed resources for a healthcare technology system to be deployed. How many items are operating in a stand-alone fashion even though there is an IT integration solution possible? Time and time again, hospitals will purchase equipment with the expectation that it will smoothly deliver data into the patient’s EHR, only to find out after the fact that the current IT environment prevents it, or that the right options were not purchased. A failure for the organization to engage biomedical equipment professionals will nearly always result in a failure to achieve optimized performance of medical devices and systems. And this costs money, money that is increasingly scarce in the world of shrinking Medicare reimbursement rates and budget shortfalls.
What is the impact on the clinical engineering department? If you are not fully engaged, if you are not a readily available asset on the C-Suite’s radar, and if the types of mistakes above are allowed to happen, you will be less likely to get the bodies you need, less likely to get the schools you want for your team, and you may not even get the equipment you need to perform the duties of your job. If you are not fully engaged and actively saving your hospital money, you are opening yourself up to be viewed as simple overhead.
Conclusion
The disconnect between the C-Suite and many healthcare technology management departments persists today. There are no immediate solutions to the technological divide, the publication problem, or the lack of administrator education. It is up to each clinical engineering department to advocate and educate our organizations. Each department has a responsibility to itself and to its stakeholders to add value to their healthcare system. The future is what we make it. Nobody else will lead the change for clinical engineering departments; it is incumbent upon our profession to do so. 24×7
References
1. Shi L, Singh DA. Delivering Health Care In America: A Systems Approach. 6th ed. Burlington, Mass: Jones & Bartlett Learning; 2014.
2. Dickey DM. Clinical engineering helps reduce equipment costs. Healthcare Financial Management. 1995;49:50–53.
Valdez Bravo is a former biomedical engineering supervisor, current graduate student, and frequent contributor to 24×7. He would like to thank John-Paul Guimond, who was an inspiration during the writing of this article. For more information, contact editorial director John Bethune at [email protected].






Valdez, thank you for this terrific article. Great resource and reminder for all of us in HTM. The current situation in Healthcare has created an amazing opprtunity for HTM professionals like never before. But, as you stated in the article – it will be up to us only how we are going to take advantage of that. And if we fail, we might consider ourself extinct(swallowed by IT departments) in the near future.
Thank you so much for the feedback, Aleksandar. Engaged, progressive HTM leaders will need to be early adopters of this new approach. I am also working to educate healthcare executives about this chasm, and hope to deliver an effective message to that audience about the power of reaching out to HTM departments in order to leverage their talents for increasing access, quality, and cost savings. Many thanks again for the note.