
Biomeds and health care facilities in general are no strangers to DAS since telemetry systems have distributed antenna systems, so although the technology may differ, the concept is the same.
There has been a lot of buzz surrounding distributed antenna systems, more commonly referred to as DAS (and pronounced dazz). Some of this buzz is well deserved: DAS do help to expand wireless coverage and can reduce the number of antennas. However, some of the buzz is due in part to excessive promotion that states a DAS solution is the “be-all and end-all” for wireless communications. The truth? Any DAS an organization chooses is not likely to be the last antenna that facility will have to install.
“When the vendors put these antennas out, they market them as the sole antenna you’ll need to do everything and that you will never have to put another antenna in your hospital,” says Tony Gwiazdowski, director of biomed and facilities for MedStar Health, Columbia, Md. “While they say that, it’s not 100% true.”
“The purpose of a DAS is to connect and combine multiple antennas into a system that provides coverage throughout a building,” says Rick Hampton, wireless communications manager with Partners HealthCare System, Boston, and co-chair for the guidance document IEC/TR 2-x:2010 Guidance for Wireless Networks. “The purpose of the ‘newer’ DAS systems is to combine the antenna systems for several individual wireless systems, such as cardiac telemetry, AT&T cellular, Sprint cellular, two-way radio, etc into one master DAS capable of serving them all.”
“So, by the strictest definition of a DAS, the discreet antenna count often increases,” Hampton continues. “But, with the newer DAS systems, you can decrease antenna count by combining the antenna systems from multiple wireless systems onto one master DAS.”
More than one DAS may be necessary or simply advantageous from a strategic standpoint, and any system can require upgrades and updating. “As technology evolves, the demands for these systems is becoming more and more challenging,” Hampton says. “So the days of a simple DAS that you install and forget about, they no longer exist. Any DAS that you buy is going to require some upgrade over time.”
However, Hampton notes that clinical/biomedical engineering departments, and health care facilities in general, are no strangers to distributed antenna systems. Although the technology may differ, the concept is the same. And so, the care and maintenance of these systems is nothing that biomed departments can’t handle. Like any other advanced technology, the systems require specialized training, but having on-site knowledge and capability is advantageous to both quality and cost.
Old Concept, New Name
“People tend to think of distributed antenna systems as something brand new, and they’re absolutely not,” Hampton says. “Every telemetry system for the past 20 or 30 years has had a distributed antenna system. It just has not been called that.” Like today’s ‘DAS,’ the older systems use multiple antennas across each floor where coverage is needed that feed back to a central bank of receivers.
“Those particular systems weren’t designed to be used to transmit signals; they were just designed to receive signals. But with a few minor changes, they could have been made to transmit as well,” Hampton says.
Today, what is typically thought of as a DAS distributes radio frequency, or RF, Hampton notes. The components are numerous and include the antennas, wiring/cabling, system infrastructure (receiving hubs), distribution blocks, splitters, controllers, switches, routers, amplifiers, and transceivers.
Different Use, Different Department
The complexity of the system will be somewhat defined by its use. “Within health care facilities, the majority of distributed antenna systems are for telemetry, but of course, they have other capabilities,” says Alan Koreneff, MBA, corporate director of the clinical equipment management program (CEMP) at Novant Health in Winston-Salem, NC.
Those capabilities can include cell phone and 802.11 wireless coverage, as well as systems such as public safety radio and emergency beepers. The decision about which systems to run on a DAS is key and one that should be addressed early on. The final menu will impact the distribution of antennas as well as who will manage it.
Often, elements of the Wi-Fi system will belong to IT departments; biomed departments will handle telemetry systems; and cell phone systems are a mix. At MedStar, biomeds handle the DAS on which the telemetry systems, cell phone coverage, public safety radio, and emergency beepers are run. “Our goal was to limit the number of antennas in the ceiling and ensure coverage throughout the hospital. We have coverage in our lobby, elevators, hallways, bathrooms, everywhere,” Gwiazdowski says.
Multiple Systems, Same Antenna (Sometimes)
The team is able to run multiple applications on the same antennas because the antennas work with multiple frequencies and systems. However, to do so requires multiple head ends (one for each application and each phone carrier). “Though we found it did not eliminate the need for multiple antennas and multiple systems, it did reduce the number of antennas we need in the ceiling,” Gwiazdowski says.
The organization decided the facility’s third-party IT provider would continue to handle the Wi-Fi system through its own network. The internal phone system, handled by clinical engineering, also has its own DAS, in part because its frequency was not compatible with the GE system, and in part because the team felt better keeping one communication system separate. “We felt comfortable that if we ever did have a crash of some sort, we would still have our internal phones, basically as an emergency radio system,” Gwiazdowski says.
Partners HealthCare System has also found that multiple DAS provide a solution offering redundancy and flexibility. “A lot of people assume, given the marketing around the DAS, that you can put everything on your DAS—and it’s true, you can. The question is, ‘Does it really make sense to do that?’ ” Hampton says. In some cases, Partners HealthCare decided it was cheaper to install multiple DAS solutions.
In general, though, a DAS is likely to cost more than a traditional system. “They’re often priced on a square-foot basis, which is much more expensive than the old systems,” Koreneff says. “So there is a large upfront cost, but there’s a lot of flexibility in the system. You’re making a decision to build for the future because everything is going wireless.”
Many Applications, One Design
Knowing what is needed from the system will be key to completing the system design. What applications will be run, and where will they require coverage? Where might expansion be needed in the future? Often, clinical engineering will work with the vendor and construction company to ensure the success of the plan. If another department such as IT is involved, it will also participate in this early preparation.
“If you’ve got a large facility, the amount of work that goes into designing and making sure that you’ve got coverage is critical. You have to make sure you have space for equipment and a place to run the lines straight up and down,” Koreneff says.
Interference among systems is not a significant problem if careful engineering is done to ensure signals are properly transmitted and the system is double-checked when commissioned. “The systems are built only to work with those applications that you connect to it,” Koreneff says. “So it’s not so much of an interference issue; it’s who’s going to own that traffic and who is going to own those applications.”
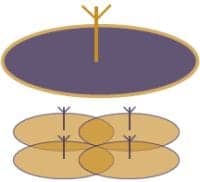
DAS systems connect and combine multiple antennas into a system that provides wireless coverage throughout a building.
One Vendor, One Process
The menu and design plan may impact vendor selection. Very often, clinical engineering’s decision regarding a vendor is tied to the telemetry manufacturer. “Selection tends to go with the vendor that you’ve chosen for your monitoring system when you’re talking about telemetry, but there also are independent companies out there that will provide a distributed antenna system, installing it and then turning it over,” Koreneff says.
However, certification that the system works properly is still required, and with a private vendor, this work will fall to the biomed department. If a problem arises, there could be a lot of back-and-forth to find a solution. Most departments have found it easier to go with their vendor, in many instances Carescape Enterprise Access by GE Healthcare, Waukesha, Wis. When Gwiazdowski searched for a vendor 5 years ago, GE was the only company with installations that could be referenced.
Using an experienced vendor can also help to facilitate the transition from an older telemetry system to a newer one. “Before you turn on the new system, you have to turn off the old one, and hospitals are not used to being without a telemetry system for days at a time,” Koreneff says. Managing the process becomes a huge project that requires collaboration with other departments, particularly nursing.
“GE has gotten much faster and can get it done in 2 days, but that is still an extremely long time to be without a centralized monitoring system,” Koreneff says.
Many Demands, Many Skills
In general, the larger the facility, the longer the time line, but Koreneff suggests departments expect about a 6-month project. “Once you sign the PO [purchase order], there’s a team that comes to work with you on the design and coverage, which takes time. Then, they start installing cables and fiber runs and everything, which easily takes 2 to 3 months,” Koreneff estimates. After that comes testing and implementation, which will require about 2 weeks of on-site activity, preparing for certification.
Service and maintenance can be arranged in typical ways, from paying a third party (vendor or otherwise) to manage the system, or handling the work in-house, oftentimes through a shared-service agreement. MedStar will be implementing this type of contract after its first-year warranty is up. “The vendor will walk us through the first PM [preventive maintenance] together, and then we’re on our own for the next 4 years,” Gwiazdowski says.
The continued maintenance requires specialized training, which, depending on the system, can be very dissimilar to previous experiences. “The week course was very different than most GE classes. You need to understand that it’s a new technology,” Gwiazdowski says. Fiber optics require specialized care, as even a simple fingerprint during troubleshooting can shut the system down.
Service can be complicated by the applications carried. For instance, if cell phone coverage is included, carriers may have their own requirements; there may also be FCC regulations that come into play when making adjustments.
“The chances are the typical biomed shop is not going to have the equipment necessary to referee any arguments that might arise when one carrier puts more power into the system than another carrier. Rather than hard-core technical skills, you’re going to have to have some managerial skills,” Hampton says. These may also come in handy when trying to work with the various parties to determine where a problem actually originates.
More Technicians, Less Downtime
Ideally, more than one person on the clinical engineering team will be able to handle issues with the system. Because it is imperative, timely service is a must. “This is something that has to run and run all the time,” Koreneff says. “If there’s a problem, the hospital is going to call the locally employed, on-site clinical engineering program.”
Full-service contracts do provide for coverage, but response time can be 2 to 4 hours, a period of time that is unreasonable for clinical teams. So the knowledge has to be on-site. In addition, parts have to be on hand, which can be a bigger challenge than expected.
“There are so many parts to these systems. The backup parts list is more comprehensive than if you were just doing telemetry,” Gwiazdowski says. Many shops wisely negotiate to have imperative parts kept on-site.
“It’s also not just having that component. It has to be programmed and set up to work with that system. So we have preconfigured components that we can just plug and play in order to limit downtime,” Koreneff says.
Thus far, the DAS systems have proven to be fairly reliable. After a year of working with MedStar’s DAS, Gwiazdowski does not expect the solution to require a full-time dedicated employee, though he does expect to have additional technicians trained to work with it, primarily to ensure uptime.
Although there is a lot of buzz surrounding DAS solutions, with communication and monitoring systems tied into their performance, they deserve the attention. And with the advantages they bring to expanding wireless coverage and limiting components, they also deserve attention. But clinical engineering departments looking at these systems should stay smart, plan well, and don’t believe the hype.
Renee Diiulio is a contributing writer for 24×7. For more information, contact .




