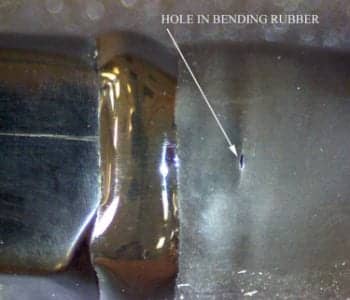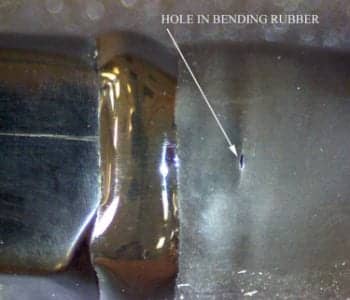
Visually inspect probes regularly and note any physical defects, such as holes in the bending rubber, indicated here.
From screening to diagnostics and therapeutic intervention, the reliance on ultrasound technology is escalating in the health care system, putting greater demands on the sophisticated equipment as well as the sonographers and echocardiographers who use it every day. Now more than ever, proper care and a proactive asset management plan have become necessary to not only preserve imaging for optimal patient care, but also to avoid downtime, costly repairs, and early replacement of probes.
The first step to protecting your image and the bottom line is simple: Proper probe care. Considering upward of 70% of all ultrasound service calls are probe related, it pays to consider ways to reduce preventable probe damage in order to minimize patient risks, and also realize the added bonus of lower costs. Studies have shown about one out of every four probes has some type of physical defect or performance problem needing resolution.1 If those defects are discovered early enough, three out of four can be repaired. Repairing versus replacing can deliver a cost savings as high as 75%—considering that repairing a probe can cost as low as $500 to $600, while a replacement can range from $7,000 to $70,000.
Proper probe care, a key factor, consists of early detection through a proactive approach to regularly inspecting probes, and resolving problems as soon as they are found. Proper probe care can be achieved by taking a few simple steps.

A $2 bite guard can prevent expensive repairs and replacements due to scratches, shown here on the tip of a TEE probe, from bites and/or tooth drags during probe removal.
Education and Training
Many who handle probes on a daily basis have never had the opportunity to see what is inside the plastic and rubber case housing the heart and soul of the ultrasound imaging chain. A peek under the probe cover reveals a sophisticated array of piezoelectric crystals (anywhere from 64 to 2,500 of them!) as fragile as glass, connected to the ultrasound system through a bundle of up to 256 tiny coaxial wires as thin as a human hair. In addition to these fragile electrical components, some specialty probes, such as transesophageal echocardiography (TEE) probes and 3D/4D probes, have intricate mechanical assemblies susceptible to damage during handling and the disinfection processes. Understanding the complexity and fragility of the internal components helps users and maintainers understand how easily these probes are damaged, and why it is so expensive to repair or replace them. By the same token, when you realize how unnoticed or unreported probe defects have potentially disastrous consequences, it is easy to see why proactive probe care is so important. So the best first step in probe care is educating yourself on the sophisticated equipment. Whether attending on-site training or taking an online course, getting familiar with the makeup of the technology can go a long way in preventive care of the equipment.

Upward of 70% of all ultrasound service calls are probe related, such as a crack in the probe case.
Proactive and Regular Inspection
The easiest part of the process is using your eyes, along with some common sense. Visually inspect probes regularly and note any physical defects, such as cracks in the probe case, nicks, holes, or worn corners in the lens membrane, cuts or tears in the probe cable or strain relief, and bent or missing pins in the connector. These conditions are usually repairable, but if left unattended they all lead to probe failure. Cracks, holes, and cuts allow fluids, such as gel, disinfectants, or even body fluids, to infiltrate the probe. When fluid comes in contact with internal electrical and mechanical assemblies, it short circuits PCB boards, causes corrosion, and damages crystal arrays.
Fluid infiltration is the biggest killer of TEE probes, often destroying them from within. These cracks and holes also allow the potential for cross-contamination, putting your patients and your facility at risk. As defects are discovered, make arrangements to have the probe evaluated for possible repair. Identifying and resolving these defects early can lower your risks, prevent more costly repairs or replacements, and save tens or even hundreds of thousands of dollars annually.
Nowhere is this more critical than in the inspection, care, and handling of TEE probes, which are used for transesophageal cardiac studies. TEE probes are extremely complex, very fragile, and are susceptible to all kinds of damage, both during a procedure and in the process of cleaning and disinfecting the probe following the procedure. These probes also happen to be the most expensive ultrasound probes in your facility and become real budget-busters when they incur damage. Here is where an ounce of prevention can prevent a ton of cure. For example, a $2 bite guard can often prevent an $8,000 repair or a $28,000 replacement. However, those figures pale in comparison to the patient risks and potential facility liability issues involved when probe defects go undetected or are ignored and the probes are kept in patient service.
A case in point: In May of 2006, a large hospital reported an outbreak of E. coli infections in nine cardiac surgery patients occurring shortly after surgery. During the investigation, a TEE probe with cracked surfaces was identified as the source of the outbreak. The cracks in the bending rubber and other probe surfaces harbored bacteria, allowing them to be transferred from one patient to the next, resulting in the infection outbreak. The hospital staff visually inspected the other TEE probes at the facility and found others had evidence of erosion not previously reported, and the additional defective probes were immediately removed from patient use. Fortunately, all the affected patients responded to antibiotics and survived the infection.2 The patients and their families avoided an unnecessary catastrophe, and the hospital clearly dodged a potential litigation bullet.

Visual inspections should include looking for cuts and tears in the probe cable.

A hole in a probe’s lens can affect the quality of the image. Holes also allow fluid infiltration, the biggest killer of TEE probes.

Bent pins in the connector are usually repairable, but if left unattended they can lead to probe failure.
Unlike the probes themselves, proactive probe care is not complex, although it is hard because it involves changing behavior and that represents the biggest challenge. After all, it only takes a few minutes to properly inspect, disinfect, and store probes. Invest a few minutes inspecting your probes, and you will provide better patient care and save a lot of money.
Probe Asset Management
More than 90% of all ultrasound failures can be cost-effectively repaired if detected early enough. The key to early detection is not only proper care. Having a maintenance strategy or a probe asset program in place will help anticipate repairs. In most cases, probe defects are not addressed until it is too late, such as when a probe suddenly quits working or the image quality slowly degrades to the point where it is no longer clinically acceptable. Then a mad scramble ensues to have a replacement probe shipped for next-day delivery so patient throughput is not interrupted. Now you are at the mercy of the market. You can buy an expensive new probe from the OEM, roll the dice and buy a “used” probe from whomever has the lowest price, or begin calling repair vendors to see which one can have a loaner probe at your facility the next day. Not exactly the best way to select who will try to repair your expensive, complex probe or sell you a “refurbished” replacement.
The cost of this reactive approach to probe management is hard to quantify, because it involves much more than the actual cost of the replacement probe or the probe repair itself, which may average $1,200 to $1,500 for standard probes and $5,000 to $7,000 for the more complex TEE probes. In addition to these “hard” costs, you also have to consider the cost of unnecessary service calls, lost revenue due to equipment downtime, staff and patient frustration, and potential negative impacts on patient safety and outcomes. These additional “soft” costs may actually double or triple the negative impact on your bottom line. Somewhere between the time when a probe is brand new and when its performance has deteriorated to the point where it has to be taken out of service, you begin to lose data critical to a proper diagnosis.
For example, the previously cited journal article demonstrated that just a few defective crystals in the array of a cardiac or vascular probe may cause a significant change in the Doppler results. This inaccurate data stemming from a hidden probe defect potentially leads to an equivocal study, and may cause a physician to schedule unnecessary additional imaging tests on a healthy patient, such as a cardiac catheterization, a more invasive procedure associated with much higher risk and cost. The primary goal in managing your ultrasound probes is to find and solve problems before they negatively impact patient management decisions and outcomes. If you do that, you will save money in the process.
There are undoubtedly probes in every hospital that are defective and underperforming. Some of them are putting patients at risk. Someone in the biomedical/clinical engineering department needs to take the initiative to develop a probe asset management program that will determine a proactive maintenance schedule and plan for repairing and replacing defective or damaged probes. This will aid in getting the problems addressed earlier, before patient outcomes are negatively impacted and when the defects are less costly to resolve. Given the current need for cost reduction without negatively impacting patient care, a proactive probe asset management plan is proven to provide a great return on investment. Several Midwestern hospital groups have realized cost savings of over $250,000 on their annual probe expenditures, resulting from proactive probe management programs.
The bottom line: developing a probe asset management program that involves proactive probe care and a repair versus replacement strategy can protect your image while saving time and thousands of dollars.
Joe Masek, MS, BS, transducer operation sales manager, Axess Ultrasound, Indianapolis, has more than 25 years’ experience in imaging equipment technology. Among other roles in ultrasound probe testing, repair, and quality assurance, he has developed proactive probe management programs for large hospitals and multiple hospital IDN groups. For more information, contact .
References
- Weigang B, Moore G, Gessert J, Phillips W, Schafer M. The methods and effects of transducer degradation on image quality and the clinical efficacy of diagnostic sonography. J Diag Med Sonog. 2004;20:395-405.
- 2006 Special Studies. (2006). Transesophageal echocardiography, insufficient cleaning practices and lax equipment maintenance, and Escheria coli—a breakdown in infection control. Los Angeles: Acute Communicable Disease Control Program—2006 Special Studies Report. Los Angeles Department of Public Health.