‘We Are All in This Together’
The biomedical engineering team at Holland Hospital in Holland, Mich, follows the patient-first philosophy every HTM professional lives by. They are also dedicated to their hospital’s overall mission to have a positive, supportive impact on the community it serves. In fact, when they’re not busy ensuring maximum uptimes for medical machines clinicians rely upon each day to treat patients, you may spot one or all of them participating in multiple charitable events, from helping raise money to feed hungry kids to lacing up their sneakers for a 5K walk to support school nurses.
Below, Jeffrey Ruiz, biomedical engineering manager—who, incidentally, took it upon himself to begin teaching potential new BMETs at the local community college when it became clear that educational opportunities are limited for hopeful HTM professionals—sits down with 24×7 Magazine to discuss why giving back, be it replacing an ultrasound probe, supporting the hospital’s EHR upgrade with a new system that included medical device integration, or jumping into action to fix a critical piece of equipment that has gone down minutes before a life-saving operation is planned to begin, is just part of the “never say ‘no'” approach this team brings to the job each day.
24×7: Can you please tell us a little bit about your team and the workload you handle?
Jeffrey Ruiz: Holland Hospital’s vision is to be the preeminent standalone hospital in western Michigan, as measured by benchmark customer service, business growth, financial performance, and clinical excellence. Our vision is honored by consistent quality awards, including being included among Healthgrades’ Top 50 hospitals each of the past three years. To help support this vision, our Biomedical Engineering team does whatever it takes to help clinical staff and physicians be successful in caring for our Lakeshore community.
Our team comprises of one manager, one supervisor, five BMETs and one ISE. We have very diverse backgrounds and experiences, ranging from those with extensive years of expertise to those who are recent graduates of the Muskegon Community College program where I teach. Our supervisor actually was born in the hospital, began his career in food service, and then joined the biomedical engineering team.
We will typically receive up to 20 service calls a day and we will complete 600-1,000 work orders per month (this includes both correctives and scheduled work). With the diverse background, it’s not uncommon for our BMETs to assist our ISE with some networking support, or for the ISE to assist a BMET with electronic board troubleshooting on a device. The culture of the team is that of working together to benefit our clinical teams. When it’s all said and done, we are all in this together. You never know when a device may be connected to a loved one.

The CE team at Holland Hospital, Holland, Mich. From left to right: Anthony Hickerty, BMET Supervisor, Jeffrey Ruiz, Biomedical Engineering Manager, James Sutliff, BMET3, James Bongard, BMET1
Michael Hopkins, ISE3, Benjamin Baird, BMET, and Kevin Heck, BMET1. Not Pictured: Tevin Eubanks, BMET1
24×7: How has your department evolved over the past few years, and how do you see it evolving even more in the future?
Ruiz: With the teams’ “never say ‘no’” attitude, we accepted an opportunity in 2013 to support the hospital’s EHR upgrade with a new system that included device integration. Typically, most hospitals will start device integration projects one modality at a time. We actually integrated six different modalities, including anesthesia machines, infusion pumps, and ventilators. This challenging implementation meant learning new systems, complex networking, and system interconnectivity. We already knew we had the device expertise, so we worked on developing the skillsets for device integration.
We still get service calls to look at SpO2 sensor or BP cuff issues, but we also now get those “CE-IT” requests for devices not sending data, or devices not connecting to our nurse notification system. Our collaborative relationship with the hospital’s clinical teams makes us the key partner for the first response on these types of service calls. Our team may not solve the service call at the point of care, but they will help facilitate a resolution with the systems knowledge of who and when to reach out to. This could be between our vendors and our IT team.
Additionally, over the years our team has strengthened its relationship with the hospital’s IT department. As our skill sets have evolved, and as devices became more interconnected, our collaboration with IT greatly increased. With the additional focus on cybersecurity, it made sense for our team to now fall under the IT umbrella. This really makes sense as it is helped streamline processes and enhance the collaborative relationship that has already existed between the two departments.
Also, we have worked very closely with senior leadership in identifying key capital replacement strategies. This had helped position the hospital to stay on the leading edge of technology and help these new devices integrate with our current infrastructure.
24×7: What would your HTM team say are probably the biggest challenges they face day to day? Can you think of an example of how they overcome or workaround the challenge(s)?
Ruiz: One of the biggest challenges is managing and servicing the various systems. When devices were standalone, it was pretty straightforward on the troubleshooting process to get the device back up and ready for patient use. In today’s world, additional layers from the multiple systems could be impacted by one device. We’re talking EHR systems, nurse notification systems, central alarm and/or management consoles, and various PACs.
Today’s vendors are so focused on being the best at what they do that, when it comes time to interface with other systems, unexpected issues arise. It becomes a challenge to solve for these “system integration” issues. To help alleviate any surprises, we have learned to add additional questions on the front end of the capital acquisition plan. Instead of saying “can you connect to this EHR,” we look at how connections happen and provide the detailed integration work plan so we can vet how the new system will integrate with our existing systems.
Maintaining an inventory with no scheduled maintenance (SM) devices also posed a big challenge. We have seen over the past few years where non-SM devices may move from one location to another. Additionally, we have seen departments acquire a device without our team’s knowledge. We tried implementing various “sampling” strategies, but none gave the results the hospital desired. That left it to us to add annual scheduled inventories for all departments and offsite locations. This gave us visibility of what devices we have left and what new devices needed inspections. We have seen great success in this process, which has also revealed some key safety concerns and process improvement opportunities, such as developing off-site device transfer policies.
24×7: Can you please discuss a time when your team “saved the day” for another department or another anecdote about the important work your team does every day?
Ruiz: The team has been very resourceful in providing key solutions that helped minimize negative down times. One such example was when we moved our backup anesthesia machine from the hospital to the Ambulatory Surgery Center when the ASC’s anesthesia machine had a hard failure. We also helped move a portable x-ray machine from the hospital to our Urgent Care location when their x-ray room had a hard failure.
Additionally, our team was quick to help set up a temporary manual cart washer while we worked on a fast-track replacement of the hospital’s current washer. We also developed a door-countering system that provided data points for the hospital’s reduction in infection rates. In each of these instances, we always focused on what we could do to address the issue, and how we could reduce negative downtime for our patients.
24×7: Is there anything else you would like to share about your team and what sets them apart from others with 24×7 Magazine’s readers?
Ruiz: One of the unique attributes of our team is the willingness to flex schedules to maintain a positive impact on patient care. This could be as simple as performing PMs during the weekend or night or having all hands on deck in collecting devices for a recall inspection. Our team is flexible to handle anything that helps the hospital succeed. This includes support for any downtime events, hospital-wide network upgrades, patient monitoring system updates, EHR upgrades, or supporting a medical gas shut down for a construction project.
Our team really enjoys giving back. Holland Hospital’s mission, to continually improve the health of the communities we serve in the spirit of hope, compassion, respect, and dignity, empowers us to give back by volunteering. The team has volunteered at our local Kid’s Food Basket – a charity that helps provide lunches for those children in need. We’ve also participated in the hospital’s School Nurse 5K Walk/Run which raises money to help fund nurses working in K-12 schools in our community. These examples really show the embodiment of our team’s culture and that of our hospital and community.





Holland Hospital in Holland Michigan. Not Muskegon. (picture Caption)
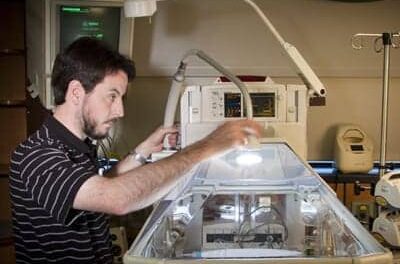
Ben Baird is a BMET1 (picture caption)