Linear accelerators are highly complex and have historically been serviced by OEMs. Why in-house support matters and how blended service models help ensure safe, reliable cancer care.
By Alyx Arnett
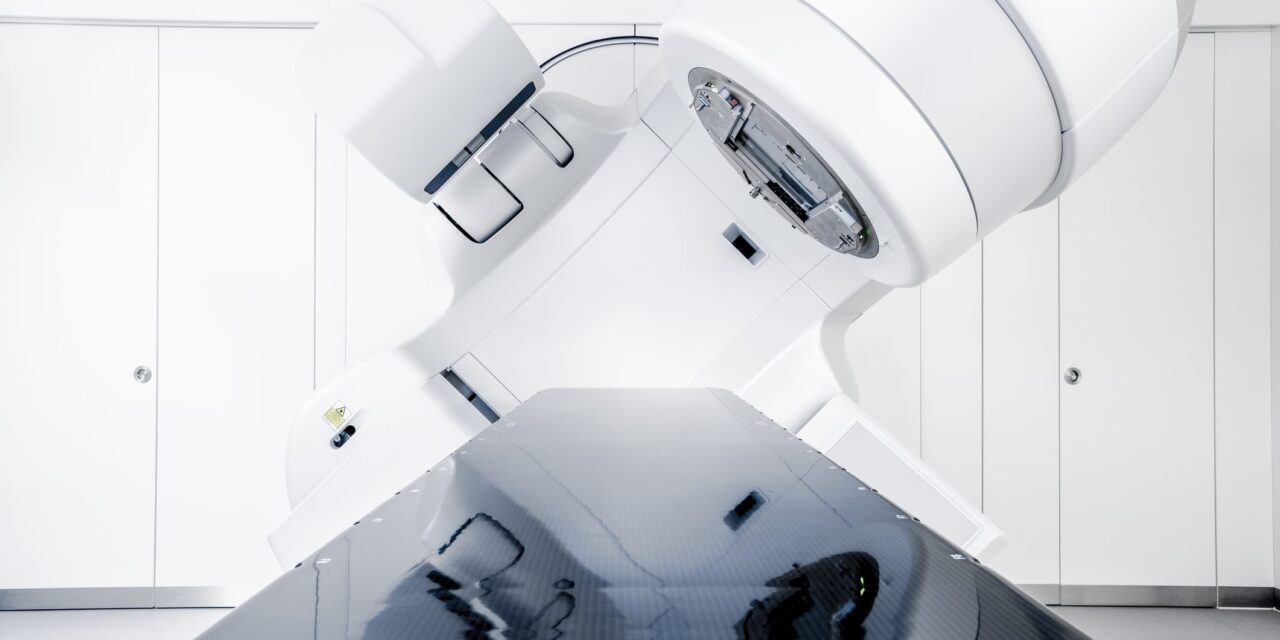
Linear accelerators (linacs) sit at a unique crossroads in healthcare technology: They are simultaneously routine and rare. Routine, because thousands of patients pass under their beams every day for cancer care. Rare, because few hospital devices combine so much physics, high-voltage power, cooling, software, and safety—and rely on a service model long dominated by original equipment manufacturers (OEMs).
For healthcare technology management (HTM) leaders, the stakes are clear. When a linac is down, treatments halt. There is no “loaner” that can roll down a hallway to fill in. “About 30 to 40% of repairs are minor, but their impact is significant because downtime is downtime,” says Alan Moretti, vice president of strategic business development at Radiology Oncology Systems. “The ability to have resources that can quickly be inserted and can triage and bring resolution is really significant.”
As cancer incidence grows and more technologies come to market, the service landscape around linacs is evolving.1 New training programs, including a vendor‑neutral curriculum delivered through the College of Biomedical Equipment Technology (CBET) with content from Linax Technologies and Radiology Oncology Systems, aim to expand the pipeline of technicians with linac expertise. “Developing a strong HTM workforce with expertise in linear accelerator training is not just a technical need; it is a patient safety imperative,” says John Vano, president of Radiology Oncology Systems.
What Makes Linacs Different
Modern medical linacs emerged as a safer alternative to cobalt‑60 machines, which relied on sealed radioactive sources to deliver therapy, Vano explains. Linacs generate high‑energy beams electrically—producing radiation when powered and stopping when powered down—and brought a new level of control and safety to external beam radiation therapy.
Yet that safety and precision rest on a complex chain of systems. From an engineering standpoint, a medical linac is a particle accelerator—technology that once lived in physics labs—in a hospital wrapper. The beamline includes electron guns, waveguides, radiofrequency power generation, vacuum systems, steering and focusing magnets, dosimetry, and multileaf collimators (MLCs) to shape the beam. Each subsystem interacts with others, and small adjustments upstream can create ripple effects downstream in ways that are not always intuitive.
“It’s not rocket science, but it is a particle accelerator,” says Marco Carlone, PhD, founder of Linax Technologies. “The beam line has many components, and the way they work together is not always easy to understand and explain. If you change something at the beginning of the beam line, you can damage the machine or miscalibrate it. That’s one reason it’s hard to learn by trial and error on a live linac.”
The devices also embed extensive safeguards. Interlocks monitor everything from door position to water flow and subsystem status. When conditions drift outside allowed parameters, the system faults by design to remain safe, often in ways that mask the underlying cause. “These machines are designed to be very, very safe,” Vano says. “A good engineer is familiar with the different faults and knows how to back‑test what might be contributing to the issue.”
The Service Landscape: OEM Dominance and a Growing Skills Gap
Linacs remain one of the most OEM-dominated technologies in healthcare, according to Moretti. “There are third‑party service companies and a segment of equipment owners with internal staff,” Moretti says. “But if we looked at it from a top-down, [service is] still very highly OEM dominated.”
Over time, service has become a major profit center for manufacturers, shifting much of the work that hospital biomeds once handled back to the OEMs. Today, most linacs are serviced by the manufacturer. The challenge, Moretti says, is that as these systems age and OEMs declare certain models end of life, support can end—creating “a growing need for engineering that can support aging equipment,” Vano says.
He adds, “When you couple that with the shortage of engineers, it puts a lot of pressure on small, especially rural hospitals that rely on older equipment. If they can’t get parts or service and can’t afford a brand‑new machine, they really could use additional HTM support and engineering help.”
A Multidisciplinary Skill Set—Plus Bedside Manner
What does it take to be an effective linac engineer? A little of everything—and then some, says Vano. He points to five domains where technicians must be knowledgeable: radiation physics, high‑voltage electrical systems, software and networking, fluid cooling and water systems, and communication.
“You’re dealing with radiation, so you almost have to study a little physics and really understand the dynamics of what is going on with the machine. The radiation is generated by a whole electrical system, so you need to be an electrician or have electrical engineering knowledge,” he says. “You need to be a little bit of a software engineer because everything is now driven by software. The water systems require a little bit of plumbing expertise because you have to know the cooling system and the water system. And then because you’re interfacing with the clinicians…you need a special skill almost like a therapist to keep everyone calm, to keep everyone understanding what the issue is.”
Those communication skills matter as much as technical mastery, Moretti says. When dozens of scheduled patients are waiting, HTM professionals become the first, most visible problem-solvers in the room. “Customer service—being able to communicate effectively and efficiently with the radiation therapists and many times the radiation oncologist—is paramount,” Moretti says. “If that factor is not there, it will quickly deteriorate the confidence level of the clinical team.”
Vano agrees. “Just like physicians have bedside manners, engineers do as well,” he says. “We’ve seen engineers who weren’t as qualified but with great bedside manners, and the customers loved them. You can’t overemphasize the importance of that skill set.”
Downtime Patterns: Many Small Fixes, A Few Big Ones
When a linac goes down, the causes usually fall into two categories: the many small faults that halt treatments and the rarer, more complex issues that demand deeper expertise.
Moretti estimates that roughly one‑third to two‑fifths of disruptions fall into the “minor” bucket—issues in controls, handsets, small electromechanical components, or software that require quick triage and restoration. They may be simple to address, but they halt patient care all the same. “The ability to quickly insert resources—on site or remotely—matters,” he says.
Vano highlights one particularly common fault: failures in MLC leaf motors. During treatment planning and delivery, dozens of small tungsten leaves shift constantly to shape the beam around a tumor. Each leaf has its own motor. “If you’re treating 35 patients a day, those motors are going back and forth all day long, so they tend to fail,” he says. “It’s a minor repair, but if one of those motors fails, the whole machine is shut down.”
Major repairs—vacuum system issues in the accelerator guide or faults in radiofrequency generation, for example—constitute a smaller slice, perhaps 10% of events, according to Moretti. These failures often require specialized tools, parts, and higher‑level skills.
Together, the two patterns help justify a blended support strategy: strong first‑call capability on site or nearby for rapid resolution of common faults, paired with deeper expertise available regionally or through the OEM or an independent service organization (ISO) when needed.
Bridging the Training Gap: A Vendor‑Neutral Pathway
Those failure patterns highlight why foundational training matters and why structured, vendor-neutral education has become a priority. Historically, linac service training has been OEM‑centric and based on the vendor’s own models. That leaves a gap for HTM teams seeking broader training or for health systems that want to develop first‑call response capacity regardless of model.
Recognizing this gap, Carlone created a simulation-based training program in 2020, and over 60 people have gone through it globally. That program—building from fundamentals of linac physics and operations through deeper navigation of subsystems and troubleshooting—is now being used in the new linac training program through CBET in collaboration with Radiology Oncology Systems. It launched on Sept 1, and early cohorts are now moving through the program.
“The goal is to provide a foundation that allows technicians to be intelligent in this area, without having to rely solely on ad hoc experiential learning,” Carlone says. He draws on a career that spans linac manufacturing and installation in the 1990s, followed by decades as a clinical medical physicist. That dual perspective shaped Linax’s simulator-centered approach to training.
One challenge in linac education is the narrow operating range of live systems. Small missteps can force lengthy recalibrations or risk damage, making it impractical to “learn by doing” across the full range of operating conditions. “With the simulator, you can change parameters in a very wide range and observe,” Carlone says. “But you also need structure. Otherwise, with so many degrees of freedom, people don’t know where to start.”
The program’s design attempts to balance both: self‑paced modules for fundamentals, instructor‑guided sessions for complex concepts, and scenario‑based exercises that mirror real‑world problem patterns. Carlone says the intent is to shrink the time to competence. “Instead of taking two years to train somebody, we want to make it six months,” he says.
What HTM Can Do Now
While the pipeline of trained professionals grows, there are practical steps HTM teams can take today to support uptime. With many disruptions falling into the minor category, a knowledgeable on‑site or near‑site HTM presence can resolve issues same‑day, reducing reliance on fly‑in service and preserving treatment schedules.
Remote access, when available, can further accelerate diagnosis and avoid unnecessary escalations. “Most of the linear accelerators in the field today have some capability of remote interactions,” Moretti says. Off‑site engineers can review error logs, assess status files, and, in newer generations, perform software corrections.
Moretti also emphasizes critical thinking and situational awareness. In a radiotherapy department, technicians must triage quickly, work independently, and communicate status clearly to clinicians who are juggling patient schedules in real time. “It’s making sure everyone understands what the issue is and what the path to resolution looks like,” Vano says.
Remote access can also complement triage workflows, allowing a local tech to consult a senior engineer quickly or confirm whether a fault is likely resolvable on-site or requires escalation.
Choosing a Service Model: OEM, ISO, In‑House, or Hybrid
When weighing service strategies, context matters. New installations typically come with OEM support, while aging assets may no longer be fully supported. Budget pressures, local talent, and equipment mix further shape options.
“All three can be very good choices—OEM, ISO, or in‑house—if they fit the organization,” Moretti says. He urges leaders to convene a full decision circle that includes the clinical team, HTM, and supply chain. Uptime requirements, escalation paths, and cost structure should be evaluated together.
Vano encourages leaders to focus on people as much as contracts. “You’re really not hiring a company to service your equipment; you’re hiring an engineer,” he says. “If you’ve got a great engineer who lives a mile down the road—regardless of what organization that engineer belongs to—that’s something you should look at.”
Both advocate for hybrid models that combine strengths: HTM first‑call coverage paired with OEM or ISO escalation; ISO where supported, OEM where proprietary tooling or keys are required; and remote support layered in across the board. “Hybrid modeling is highly successful in achieving many of the objectives organizations are seeking,” Moretti says.
Emerging Pressures: Keys, Workforce, New Tech, and Rural Access
Looking ahead, several trends are shaping how linacs are managed.
First is the expanding use of software keys and access controls that restrict servicing to manufacturer pathways. “OEMs are trying to protect their technology by using software keys to lock out the ability to service equipment,” Vano says. He notes that facilities and OEMs are actively negotiating where the boundary lies between in‑house service authorizations and vendor‑exclusive tasks. He recommends HTM leaders engage early on access provisions when purchasing and renewing contracts to ensure they can perform in-house service where appropriate.
Second is workforce. Many experienced linac engineers are nearing retirement, and few neutral avenues existed until recently to onboard new technicians. “It’s a highly important and crucial situation at this juncture,” Moretti says. Carlone adds that service contracts can run into the hundreds of thousands of dollars per system annually—an economic reality that compels hospitals to pursue internal capacity where feasible.
Third is technology diversification. After years of limited vendor competition in the United States, more US Food and Drug Administration-cleared entrants are emerging. “We’re seeing a record number of new entrants into the marketplace, new technologies coming in,” Vano says. Some of them are hybrid platforms that combine linacs with MRI or PET. As equipment diversity increases, professionals able to service these devices will be sought after, he says.
Vano also underscores access gaps for rural hospitals. High equipment costs, difficulty recruiting clinicians, and reliance on older systems often limit rural access to radiation therapy. Refurbished systems, lower‑cost service options, and local HTM upskilling can help extend therapy closer to home for many patients. “Anything we can do as an industry to help these rural clinics—and cancer patients that live in rural areas—is really important,” he says.
The Path Forward for HTM
Demand for radiation therapy—and for the linacs that deliver it—continues to rise as immunotherapies and other advances extend lives. “Paradoxically, we’re getting more patients,” Carlone says. “It’s a good problem to have, but it is a problem. We need more people who can make sure these machines work.”
Still, a challenge remains in that a sense of fear often surrounds these systems. “They’re complicated machines. They make radiation. Radiation is dangerous, and so there’s a fear,” he says. “The people who work in the industry have a really high culture of quality assurance. We don’t want to make a mistake. The last thing anyone who works with cancer and takes care of patients wants to do is harm a patient.”
Now, that culture is starting to shift. With a new vendor-neutral training program and efforts to expand in-house and third-party expertise, more professionals are learning how to safely manage and service these devices. Over time, Carlone says, that understanding could help replace fear with confidence. “The opportunity here is to get rid of the fear people have about these machines,” he says.
Reference
- WHO. Global cancer burden growing, amidst mounting need for services. World Health Organization. 2024 Feb 1. Available at www.who.int/news/item/01-02-2024-global-cancer-burden-growing–amidst-mounting-need-for-services
ID 132766078 © Thomashecker | Dreamstime.com