|
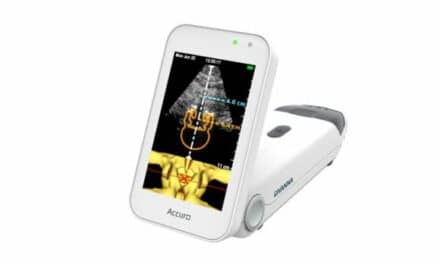
| There is a noticeable difference in the 3D/4D image when compared with the traditional 2D image, but there is not much visible difference in the equipment. |
Today, expectant parents can start the video record of their child’s life in utero. Ultrasound technology has added not only a third dimension (3D) of depth but also the fourth dimension (4D) of time. Ob/Gyn has made the most use of this technology. Roy Doyel, radiological equipment service tech with St John’s Regional Health Center in Springfield, Mo, attributes the discipline’s rapid adoption to the conducive environment of the uterus. “Because the amniotic sac is filled with fluid, it is ideal for 3D ultrasound technology,” Doyel says.
Expectant parents, however, do not have sole command of the technology. 3D/4D ultrasound is also making inroads into cardiology, where it is more frequently referred to as live 3D (volume 3D being another moniker), according to Nate Pinkney, BS, RDMS, senior project engineer with the Health Devices Group at ECRI Institute, Plymouth Meeting, Pa. “The cardiology department has expressed interest in live 3D, which provides more information about the heart and blood flow than a frozen 3D image,” Pinkney says.
But even though there is a noticeable difference in the 3D/4D image when compared with the traditional 2D image, there is not much visible difference in the equipment. “There isn’t much difference between a 2D and a 3D scanner in the hardware itself, and so there is no difference in handling the repairs,” Pinkney says.
There are different ways to obtain the 3D image, which are important to consider when purchasing the equipment. In terms of maintenance and service, the biggest differentiations are the probe and the software, which also tend to be where problems most often originate.
Doyel estimates that the biomeds at St John’s Regional Health Center handle about 70% of the ultrasound repairs in-house. He notes that a greater portion of this is hardware. “We don’t disassemble transducers and repair them because that requires a clean room, but we do handle minor repairs and exchanges,” he says. Software is trickier since vendors are often reluctant to give up this proprietary information, and software is really what provides the 3D and 4D functionality.
Higher Dimensions
“The ability to produce three-dimensional images on an ultrasound system is primarily due to software,” Pinkney says. Some scanners will produce a 3D image using the same transducer as that used to capture a 2D sonogram. “The transducer picks up slices in a single plane, which are then reconstructed into a multiplanar view,” he says.
Volume imaging, which uses specialized transducers, captures raw data that can be used to create volumetric and multidimensional images in real time as well as for later analysis. Advantages include faster acquisition and exam times. “This technological difference is a concern primarily when comparing specifications among different manufacturers. They may state 3D capability, but you need to check what they are referring to as 3D,” Pinkney says. The majority of scanners produced today, particularly at the high end, offer some type of 3D function.
Some systems build the capability directly into the system; others add it through an external box. “The manufacturers are still using the basic architecture of the traditional ultrasound system,” says Fred G. Whayn, senior ultrasound specialist with Masterplan Inc, Chatsworth, Calif.
Integrated systems will have one hard drive and display, a transducer or selection of transducers, and one power supply. External systems will have two hard drives, one display, a transducer or selection of them, and two power supplies. “You see the same components on a 3D system that you have on a 2D and can expect the same problems,” Whayn says.
Probing Problems
Whayn—who has more than 16 years of experience working with ultrasound equipment—has found transducers to be the most common cause for service, followed by software and the power supply. As probe technology has advanced, the transducers have become more prone to breakage. From the second law of thermodynamics one could infer that that which is mechanical will eventually break down. Most biomeds infer this as well, but from experience.
Some 3D probes are capable of scanning and capturing an entire area, such as the uterus, from one location on the body rather than having to physically scan the region. This requires motorized parts inside the probe. The mechanical probes are required for some 3D acquisitions and are needed for all 4D. “Once a probe contains motors, it’s susceptible to problems and will exhibit a higher failure rate,” Pinkney says.
The motorized probes are more easily damaged by physical shock, as well as extreme temperatures, than those used for 2D ultrasound imaging. Whayn estimates that the 3D mechanical transducers break down twice as often as those used to acquire 2D. “The fluid inside [the 3D models] expands and contracts with temperature changes and may leak out over time,” he says.
Exchanges are easy when backups are available, but the 3D/4D transducers are significantly more expensive than those used for 2D image capture, sometimes two or three times as much. Pinkney estimates a replacement mechanical probe runs between $10,000 and $20,000. Subse-quently, he recommends service contracts.
“This expense is not something hospitals typically want to cover, so biomeds should have some service in place designed to cover transducer replacement,” Pinkney says. “Even when they handle general repairs on the ultrasound equipment, when they need to replace a transducer, they’ll take advantage of the contract.”
“Ideally, the transducers will last the life of the ultrasound machine, but user handling can cause damage. The probes get dropped on the floor or knocked against a gurney, a cord gets yanked out while the unit is being moved,” Whayn says. He estimates that 90% of transducer failures are due to mishandling and suggests that machines with fewer users are better cared for and have longer life spans as a result.
“The most reliable systems I have seen have been installed at facilities where there are one or two people using the equipment without transporting it throughout the facility for exams,” Whayn says. Reliable for a transducer currently means a life span of about 5 years, which can be achieved if the device is cared for properly both in use and storage. A busy department may see that lifetime reduced to 3 years. “Most ultrasound equipment is outdated after 5 or 6 years anyway,” Whayn says.
Some users may opt for reconditioned transducers, but the market does not yet hold a lot of options since the equipment is still new, according to Pinkney. Whayn concurs, “No one is really touching 3D mechanical probes on the used market right now unless they are using them for minor repairs, such as refilling liquid,” he says.
Getting Onboard
The rest of the ultrasound unit is sturdier, though it can be trickier to maintain and repair. Whayn suggests that biomeds request that the manufacturer turn on any type of diagnostics at the time of the system’s purchase. They will be needed, particularly if the preventive maintenance (PM) program will be handled in-house.
“A lot of times you can’t have the diagnostics turned on unless you have been trained on the system, and you can and should negotiate training into the sales deal, when it’s easier to obtain for free,” Whayn says. After the sale, biomeds must often go through the service department and will be charged for training.
As part of the negotiations, users may have to pay a small fee—”perhaps 50 dollars,” Whayn suggests—and/or sign proprietary and nondisclosure forms. Vendors may not readily hand over the software, but “they have to give it to you,” Whayn says.
The diagnostics are particularly useful when running PMs and test objects. “To ensure the instrument is putting out the best-quality images possible, use a test object to perform the recommended preventive maintenance or inspections—paying particular attention to the transducers—at least as often as the manufacturers suggest,” Pinkney says.
Test objects provide repeatable images that help to check the system’s capabilities. “Basically, the test object is a box that holds a chunk of simulated tissue designed to represent a three-dimensional structure. Most often it’s a baby’s head or a fetus. I have heard of a heart-shaped test object but have not yet seen it,” Whayn says.
If no test object is available (those for 3D will cost about twice as much as those used for 2D testing, according to Whayn), biomeds have been known to scan themselves. “A test object is better when you want to check the 3D functions of the scanner, including reconstructions, and is recommended for troubleshooting, but a biomed can troubleshoot using his own body when trying to determine if there is a functioning problem in general,” Pinkney says.
Troubleshooting from the Hip
Most often, however, the users note troubles with an ultrasound device. “The best way to know if there is a problem is to rely on the technologists that use the equipment every day. They are your best resource,” Whayn says.
Pinkney concurs, adding, “Since these units are rarely taken out of service, it’s often the user who does notice a problem, often from images that look abnormal.” Problems can range from the intermittent to hard failure. For instance, noise issues can periodically appear on the display, or the fetus may appear to be an unusual shape and the effect is across all scans. The user often calls the biomed, who then begins a process of elimination.
“One of the best ways to determine the source of a problem is to eliminate possibilities. The process works particularly well when there are no onboard diagnostics to help,” Doyel says. He starts by checking alternate connector ports, transducers, and exam times.
Whayn also recommends trying different solutions. “You want to isolate the problem,” he says. Questions he asks include: Does it happen with one probe or all? Is it a 2D or 3D/4D issue? Does the system work in a 2D mode? Is it working properly in 3D/4D mode?
“It’s rare to have a true 3D complaint,” says Doyel, who notes that with reconstructive technology, if the 2D function is not operating, the 3D image will also be impacted. “The biomed should first clarify and address any 2D issues before advancing into 3D verification and checks,” he says.
Having an additional machine available to assist with the elimination process is ideal, according to Doyel. “When you are questioning whether the specialized transducer is functioning, you can try it on the second machine,” he says.
An Ounce of Prevention
Of course, most biomeds and users would rather avoid poorly functioning equipment altogether. PMs can help, but regular cleaning can help even more. “Anything that heats up will fail sooner,” Doyel says. “Properly cleaned ultrasound equipment will have better airflow, will run more coolly and efficiently, and will take longer to fail.”
Properly cleaned doesn’t just mean vacuuming; Doyel thinks compressed air is better. “Vacuuming is better than nothing, but it won’t get the dust out of hard-to-reach places,” he says.
After implementing a cleaning program at St John’s Regional Health Center, Doyel noticed a “huge” difference in the equipment and service calls. Even facilities with contracts will want to pay special care to make sure the equipment is cleaned, whether they do it themselves or ensure it is part of service. “The in-house biomed is the most concerned with getting the maximum performance from the equipment and therefore has the greatest incentive to properly care for and clean it,” Doyel says.
User care can also help. “Users need to be careful not to drop the probes—one of the biggest problems,” Pinkney says. In addition, they can help by noticing signs of wear so problems can be corrected before replacements are necessary.
Even if much of the equipment’s service is handled in-house, Pinkney does not expect biomeds to generally spend much time on ultrasound units. This is good news, since hospital usage of 3D/4D models is on the rise. The advanced models capable of 3D and 4D imaging require very little extra maintenance and repair, particularly when their usage (currently less than 2D ultrasound imaging) is factored in. “As long as the biomed follows the recommended preventive maintenance, there should be no significant problems. It’s not uncommon to have a scanner that doesn’t require service for a year. Systems today are very reliable,” Pinkney says.
Renee DiIulio is a contributing writer for 24×7. For more information, contact .