With disasters on the rise, HTM teams are relying on modern tools and coordinated planning to support smarter emergency response.
By Alyx Arnett
The chance of Unicoi County Hospital in Erwin, Tenn, ever flooding was just 0.2% annually, based on its 500-year flood zone designation. But that unlikely scenario became reality on Sept 27, 2024, when the remnants of Hurricane Helene swept through the region and inundated the facility.
Floodwaters rose eight feet inside the single-story hospital. Ambulance access was lost. Debris-filled currents made boat rescues hazardous, and the only way out was up. Staff and patients climbed ladders to the roof—or waited in tethered rescue boats—until helicopters could arrive. Fifty-four people were airlifted to safety.
The 2024 Super Bowl parade shooting in Kansas City presented a very different kind of emergency. At Children’s Mercy Kansas City, where 12 shooting victims—11 of them children—were treated, hospital leaders activated pre-established mass casualty and surge plans the moment the incident occurred.
While the events were vastly different, both hospitals faced the same test: how to respond when disaster strikes close to home—and in ways few saw coming.
The New Normal: A Broader, Unpredictable Threat Landscape
In 2024, the United States experienced 27 weather and climate disasters that each caused over $1 billion in damages, according to the National Centers for Environmental Information.1 That’s three times the long-term annual average of nine events per year and consistent with the sharp rise seen in recent years. From 2020 to 2024, the five-year average has climbed to 23 billion-dollar disasters per year.1
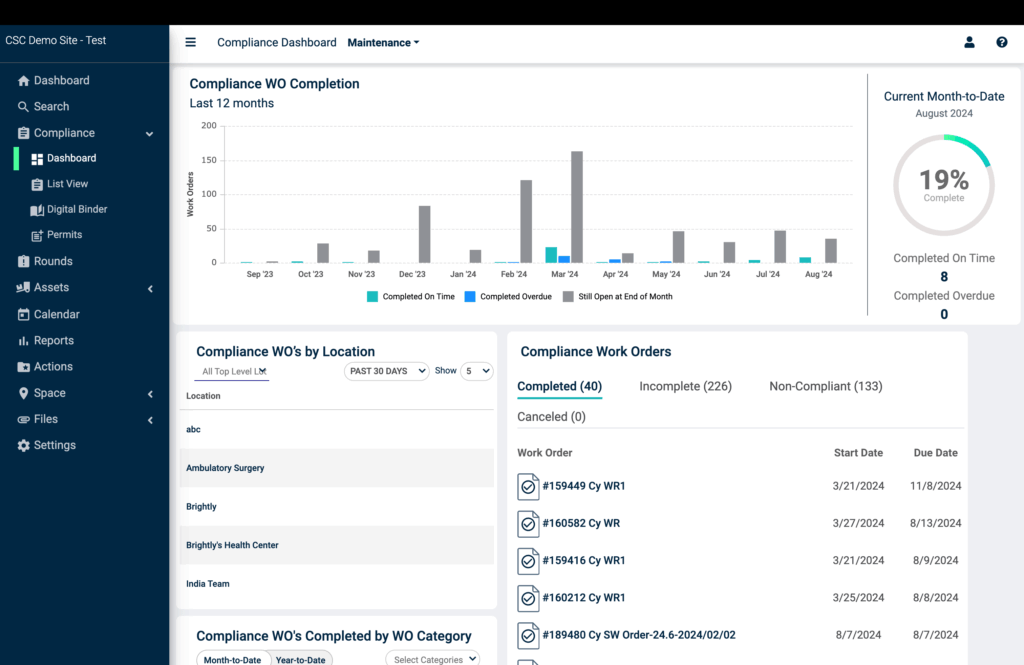
This rise in frequency and severity is placing new pressure on healthcare systems to prepare for scenarios that once seemed improbable. Mark Mochel, MBA, PMP, CSM, FCT, ACABE, strategic account executive at Brightly Software, a provider of computerized maintenance management systems (CMMS), points to recent examples: hospitals in the Southwest grappling with sub-freezing temperatures and burst pipes; facilities in Tennessee and Kentucky overwhelmed by flooding; and Midwestern hospitals forced to modify air intake and filtration systems due to Canadian wildfires.
“Disasters common to one area are cascading effects elsewhere,” says Mochel. “What was once uncommon is now part of the new normal.”
Even routine disruptions are becoming more common. Summer blackouts have increased by 60% over the last decade, Mochel points out, placing critical systems—such as life support equipment, ICU infrastructure, sterilization units, and temperature-sensitive medical devices—at greater risk.2
These occurrences mean that even hospitals outside traditional danger zones must reassess their risk. “The approach to planning should be, ‘What if it happens?’ instead of, ‘That will never happen here,’” Mochel says. “Always assume the worst-case scenario, not the best.”
When Plans Become Lifelines
Ballad Health’s Unicoi County Hospital is a key example of how even regions considered low risk can be overwhelmed by sudden disaster. “We had never seen anything like this,” says Eric Deaton, COO of Ballad Health. “I think everyone felt that this region was safe from this type of flooding.”
The hospital team was able to act fast due to its Corporate Emergency Operations Center, created during the COVID-19 pandemic. The multidisciplinary team—including physicians, nurses, human resources, communications, finance, supply chain, engineering, and IT—was activated as floodwaters began to rise. “We were able to have the team together to sit and make decisions quickly,” says Deaton. He adds, “One of the first things [clinical engineering] did was turn the electricity off to the hospital.”
The 10-bed hospital used its Epic electronic medical record system to view capacity across the system’s 20 hospitals and guide patient transfer decisions. The hospital was forced to pivot from ambulance transfer to air rescue as nearby roads quickly washed out. Ultimately, no one was killed or injured in the disaster, though the hospital was deemed a total loss. In February, the State of Tennessee and the Federal Emergency Management Agency approved $9.8 million in funding to replace the facility.

Looking back, Deaton says the experience reinforced the importance of acting quickly and always being prepared to move patients. Just as critical, he adds, are strong relationships with emergency partners. “What really saved our patients and staff was our relationships with agencies,” he says, including the Virginia State Police and the Tennessee Emergency Management Agency. He also points to the value of post-event tabletop reviews to help identify ways to coordinate more effectively in the future.
At Children’s Mercy Kansas City, emergency response has been built into daily operations. Following the 2022 pediatric “tripledemic,” the hospital launched its Patient Progression Hub—a 6,000-square-foot, 24/7 operations center that tracks patient flow, bed availability, and staffing levels using GE HealthCare’s Command Center software.

The hub supported emergency response during the 2024 Super Bowl parade shooting. “They could tell us, moment one, ‘Here’s where we’re at as a hospital. Here’s what we can take. Here’s what challenges we think we’ll have,’” says Morgin Dunleavy, MSN, RN, CPEN, director of emergency management. “That was incredibly helpful for us as leaders and decision-makers when we’re talking to teams in the field or our city partners.”
Just as critical, the hub helped manage the surge of patients while maintaining visibility into the rest of the system to ensure routine care continued uninterrupted. “One piece that gets lost in the time of a disaster is you still have all patients with their normal, everyday healthcare needs. And so you may be managing a component over here that’s a disaster-related response, but you need to make sure the rest of the organization that may not be the front line of that disaster piece is running effectively and efficiently,” she says.
To further strengthen its preparedness, Children’s Mercy is working with its HTM department to evaluate how technology can better support disaster planning. “We’re doing a big initiative with them now to look at all of our systems through their lens to say, ‘Are there gaps that you know of that maybe aren’t on our radar? How can we help close those gaps for this disaster planning? What else can the technology do that we’re not thinking about or maybe don’t have awareness of as clinical leaders or operational leaders? How can technology help us?’” Dunleavy says.
Tech That Keeps Hospitals Running
Technology plays a key role in disaster response, helping hospitals maintain system continuity, track equipment, and make real-time, data-informed decisions.
Real-time location systems (RTLS) like GE HealthCare’s Encompass and TRIMEDX’s GeoSense, for example, help hospitals quickly locate assets. “From pre-staging devices to preventing loss in the chaos, these tools allow HTM teams to respond smarter, faster, and stronger,” says Rob Moorey, FACHE, president of clinical engineering at TRIMEDX.

For expected surges, RTLS “becomes very important for a hospital to identify where all their equipment is quickly, gather it, put it in a location, and get it ready for all of the patients that are coming in,” says Mohamed El-Demerdash, president of US and Canada Service at GE HealthCare.
CMMS and asset management platforms also support preparedness. “These solutions offer the ability to track operational performance of critical assets and systems, identify deferred maintenance levels, and accurately forecast future repair and replacement capital needs,” says Brightly Software’s Mochel.
During disasters when technicians can’t reach equipment, remote service capabilities can provide an alternative. GE HealthCare’s remote monitoring tools, for example, allow off-site experts to log into networked devices, diagnose issues, and, in many cases, complete repairs without setting foot in the hospital.
With some assets, up to 40% of issues can be repaired remotely. “You can imagine that, in a disaster situation, the speed of somebody being able to connect in and resolve something would be very critical,” El-Demerdash says.
Prepared to Power Through
Disaster planning demands foresight into how infrastructure, equipment, and support systems might fail. “HTM teams face issues such as transportation disruption, water damage to devices, and the inability to safely power or use equipment after flooding or power loss,” says Moorey.
When power is interrupted, even briefly, the impact on powered equipment and connected systems can be unpredictable. “That’s typically the challenge in a disaster,” adds Jeremy Ramsey, Intelas regional director of operations, providing clinical engineering services at Memorial Hermann Health System in Texas. “When the power shuts off and goes on to generator power, what is the side effect? Does the telemetry system not come back up correctly? Does the MRI system not come back online and continue scanning?”
In these moments, checking the backup systems and battery reserves becomes essential. “They’re going around validating that the backup power systems are operational and making sure batteries aren’t depleting,” Ramsey says. “If they are, then they’re working to swap those out to keep things powered up and running.”
Derrick Johnson, senior vice president and chief operating officer at Agiliti, recommends having options to manually operate equipment when needed.
Staffing can also pose another challenge. Ramsey recommends triaging calls based on equipment criticality. “If you’re a stroke hospital and your CT is down, that CT needs to be up and running before your TV in your patient room,” he says.
Some hospitals also partner with outside service providers to prepare for and respond to equipment surges. TRIMEDX’s Mobile Medical Equipment program helps hospitals stage and manage essential devices—such as ventilators and infusion pumps—ahead of major storms. Agiliti offers complementary surge capacity through its national rental fleet, often stepping in during acute disasters. During Hurricane Beryl in 2024, Agiliti teams worked alongside hospitals in Houston to retrace orders, stage equipment, and support HTM departments, according to Andrew Yamarick, general manager of medical technology management at Agiliti.
HTM service partners are often integrated into emergency preparedness plans. At one Florida hospital, an on-site TRIMEDX team rode out a hurricane, protecting equipment by covering CT scanners and other sensitive devices in plastic, moving equipment to higher levels, and filling sandbags to guard generators. “Our HTM teams had prepared ahead of the storm, dividing up into a team that would stay at the hospital through the storm and others that would relieve them when it was over,” says Moorey.
Integrating HTM into Disaster Preparedness
The Joint Commission requires healthcare organizations to have an emergency preparedness committee responsible for developing and implementing an emergency management program. While the standards don’t mandate specific committee members, Rebecca Crossley, a TRIMEDX-contracted BMET III at UPMC Williamsport in Pittsburgh, says HTM must be included. UPMC Williamsport has had an HTM member on its committee for at least the past decade, Crossley says.
That need is emphasized in AAMI’s HTM Emergency Preparedness Guide, published in 2021 in response to the growing number of events disrupting healthcare delivery. Developed by members of the AAMI Technology Management Council—including Crossley—the guide outlines HTM’s role across all phases of disaster response and provides practical tools for integrating teams into system-wide preparedness efforts.3 “Any emergency response will ultimately affect equipment and patient safety, and HTM has a critical role in this response,” the guide reads.
Key elements of the guide include:
- Emergency Preparedness Assessment Tool: A checklist to evaluate HTM readiness across staffing, supplies, and communication systems.
- Continuity and Compliance Templates: Tools to prioritize departmental tasks and manage scheduled maintenance during emergencies.
- ICS Integration: Guidance for aligning HTM with the Hospital Incident Command System and establishing points of contact.
- Mutual Aid Considerations: Recommendations for managing vendor agreements and emergency access authorizations.
Crossley says the guide also helps departments advocate for greater inclusion in emergency drills and planning discussions. “I think the hospitals have plans, but quite a few hospitals just weren’t involving their biomed or HTM people in the process,” says Crossley.
Industry leaders stress that HTM teams should be part of these efforts. “It’s essential that HTM is included in capital planning, budgeting, and approval processes to ensure infrastructure and technology needs are appropriately prioritized,” says Brightly Software’s Mochel. TRIMEDX’s Moorey agrees, encouraging HTM professionals to review their facility’s emergency management plans, understand their roles, and actively participate in drills.
Photo caption: Ballad Health’s Unicoi County Hospital was declared a total loss following severe flooding that occurred on Sept 27, 2024, when the remnants of Hurricane Helene swept through the region.
Photo credit: Ballad Health
References:
- NOAA National Centers for Environmental Information. US Billion‑Dollar Weather and Climate Disasters. 2025. Available at https://www.ncei.noaa.gov/access/billions/
- Climate Central. Heat season power outages. Climate Matters. 2024 Aug 21. Available at https://www.climatecentral.org/climate-matters/heat-season-power-outages
- Association for the Advancement of Medical Instrumentation (AAMI). Emergency preparedness assessment for HTM departments. 2021.




