RTLS is no longer just about finding equipment. Better accuracy and maturing integrations are pushing location data into maintenance, capital planning, patient flow, and more.
By Alyx Arnett
Real-time location systems (RTLS) are hardly new to healthcare. What’s changing is how organizations are using them, as more accurate data and maturing integrations push RTLS beyond basic device tracking.
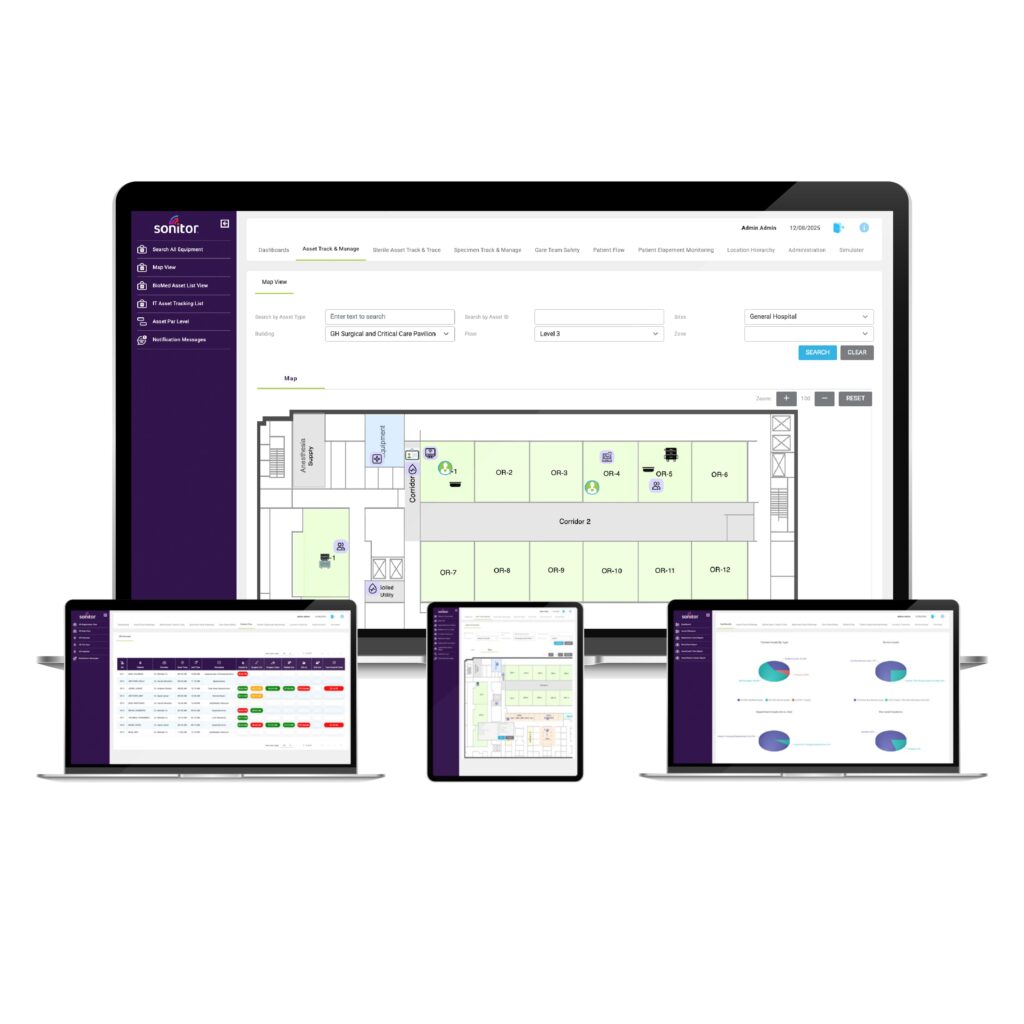
Erik Davidson, vice president of strategy and marketing at RTLS provider Sonitor Technologies, says these advances are expanding RTLS’ role into areas like asset lifecycle management. “By integrating RTLS data not only with maintenance systems but also with ERP (enterprise resource planning) platforms, hospitals can get new levels of visibility into the asset fleet,” he says.
Through integrations, RTLS is also increasingly supporting maintenance workflows, capital and inventory planning, patient throughput, and even cybersecurity efforts.
The Accuracy and Cost Equation
A key reason RTLS is moving beyond location tracking is improved accuracy, says Davidson. When location data is only accurate to the floor or wing level, RTLS is largely limited to helping staff search for equipment. But when accuracy reaches the room or bedside level, hospitals can begin using RTLS data to drive workflows and feed other operational systems.
Most early RTLS deployments relied solely on signal strength from Wi-Fi networks, which often resulted in “floor-level” accuracy, Davidson says. “That might be OK for a wheelchair,” he says, “but it is not OK for an IV pump.”
Now, vendors are increasingly addressing accuracy challenges by offering multiple location technologies—such as Bluetooth low energy, ultrasound, infrared, and ultra-wideband—alongside traditional Wi-Fi. The goal, Davidson says, is to match the level of accuracy and cost to the specific use case. “You might tag an IV pump with something that tells you exactly which bedside it’s at,” Davidson says. “But for a wheelchair, you may only need to know the department it’s in. That might call for a lower-cost tag with longer battery life, even if it sacrifices some accuracy.” For small or disposable medical supplies, teams may opt for disposable RFID tags instead of battery-powered RTLS tags, he says.
Alongside these advances, the economics of tagging have also improved. Tag prices have come down, and battery life has increased, says Wyatt Meek, chief commercial officer at RTLS vendor AiRISTA, making it more practical for hospitals to expand RTLS beyond a small subset of devices. “When hospitals did their initial deployments five years ago, tags were more expensive and often required dedicated hardware,” Meek says. “With price points coming down, it’s become more economical to track more assets.”
As a result, hospitals that once limited RTLS to a few thousand high-value devices are expanding their scope. “Let’s look at instead of just tagging those 3,000 before, let’s now tag 10,000. Let’s tag all your assets. And so that’s where we’re seeing it expand,” says Meek.
Integrations Are Gaining Traction
That expanded, more accurate data, Davidson says, sets the stage for integrations. And he says these are becoming increasingly possible as more platforms move to RESTful APIs—standardized interfaces that make it easier for systems to exchange data. This means RTLS data can be pulled into the systems technicians and clinical teams already use, whether that’s a CMMS, an ERP platform, or a device management system.
“RTLS needs to do more than just track equipment. It must seamlessly integrate into a broader clinical asset management strategy to stay effective,” says Murphy McGraw, senior director of product management at TRIMEDX.
ERP With RTLS
By connecting RTLS data with ERP systems, Davidson says hospitals can analyze usage patterns to right-size inventory, reduce unnecessary rentals, and avoid over-procurement.
He points to one example of a hospital using RTLS to monitor IV pump availability in a busy emergency department. When pump levels fall below a defined threshold, the system can trigger alerts to adjust cleaning and restocking schedules in real time, without manual intervention.
Over time, that same data can help equipment managers determine whether an emergency department consistently needs more pumps, or whether existing inventory can be redistributed from other areas, he says.
“Most RTLS users could start to go down this direction if they have the right RTLS technology in place that’s accurate enough and reliable enough, and if their systems lend themselves to integration,” he says.
CMMS With RTLS
RTLS-CMMS integration is a growing area customers are looking at, says Shawn Hewitt, senior product manager at computerized maintenance management system (CMMS) provider FSI. By connecting these systems, technicians can see current device locations within work orders, potentially reducing the time spent searching for assets scheduled for planned maintenance.
Hewitt says this can help teams reduce “unable to locate” status codes. “If you have 60% of your work orders that are in ‘unable to locate’ status, let’s set a goal that only 10% of your work orders at any given time should be unable to locate,” he says. “Through the value of the integration, we want to make sure that technicians can find their work orders. That’s so important for compliance.”
Children’s Health in Dallas, Texas, was an early adopter of an RTLS-CMMS integration, merging the systems in 2019 after realizing that tag data could be stored in the asset record. That allows technicians to access the data and look up the tag directly in the RTLS system, says Stacey Williamson, HTM director of enterprise systems at Children’s Health.
“We were focusing on giving our staff a quicker way to search for equipment and also a way to audit the data between the two systems for accuracy,” says Williamson.
Through the system, an asset’s location is updated every five minutes, and the tag address from the RTLS feeds into the CMMS, automatically updating asset records. “Overall, it’s reduced manual data entry, improved response times, and given us better visibility into asset health and maintenance performance across the operation,” says Andrea Brainard, CBET, CHTM, at Children’s Health.
For hospitals considering integrating RTLS with a CMMS, ensuring location data is accurate is critical, says Hewitt. “We caution people to make sure that your RTLS is set up in a way that it’s accurate today,” he says. “If it’s showing on the second floor in Room 508, make sure that’s where it’s really at because, when you connect to the CMMS, that’s what it will show.”
RTLS accuracy often depends on the hospital’s underlying IT infrastructure and how the system is deployed, Hewitt says. In some cases, organizations may need to strengthen network coverage or add supplemental RTLS hardware—such as additional waypoints or a vendor-provided mesh-style network—to improve reliability in difficult areas of a facility.
EHR With RTLS
Philipp von Gilsa, CEO of RTLS provider Kontakt.io, says hospitals are increasingly using RTLS data alongside electronic health records (EHR) data to improve outpatient clinic operations, including room utilization and patient flow.
Kontakt.io recently launched an AI-based agent, for example, that combines real-time location data with EHR information and historical utilization patterns to forecast room availability and visit duration. “At scale, [this] gives health systems a truly accurate picture of their ambulatory capacity by bringing together historical patterns and RTLS actuals into one real-time map,” von Gilsa says.
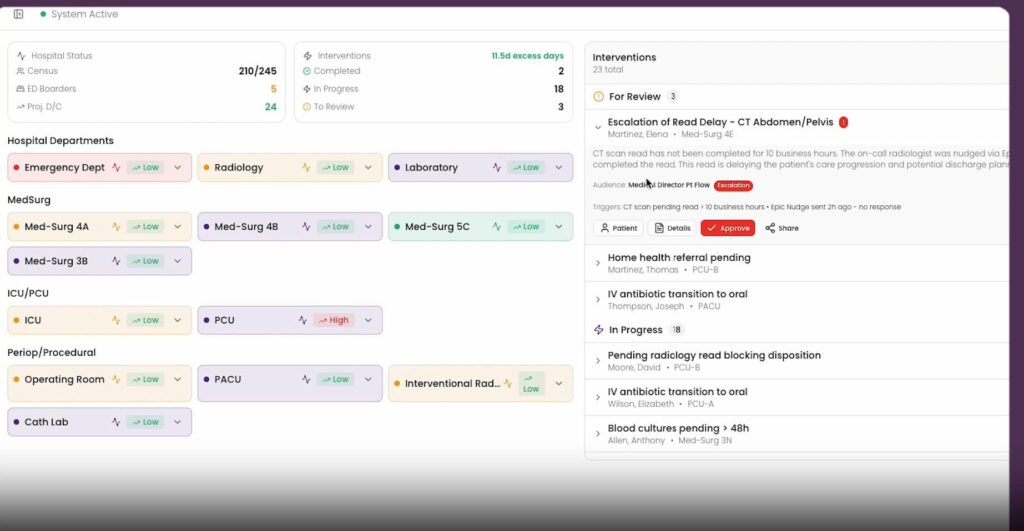
Another AI agent from Kontakt.io, currently being piloted at US hospitals, integrates EHR and RTLS data to predict equipment demand and automatically orchestrate workflows to ensure equipment reaches the right location when it’s needed.
Additionally, Kontakt.io’s recently launched Patient Journey Analytics, also being piloted at US hospitals, that combines EHR data with real-time operational inputs, including RTLS data, to create what the company describes as a “digital twin” of hospital operations, designed to support more predictive decision-making.
Expanding Integrations
RTLS integrations are extending into other areas as well. AiRISTA’s Meek points to an integration with BD Alaris infusion pumps as an example. Through this integration, RTLS can provide status data, indicating whether a pump is actively infusing, sitting idle, or has an alert.
This can save a technician from tracking down a piece of equipment for servicing only to find it’s in use, as well as streamline alerts. Meek says it also allows for better data utilization. “We know five are actually infusing. Two are out of service. Two need cleaning,” he says. “So that additional information that we can now provide with RTLS enables hospitals to be more efficient in their operations.”
For improved bed management, Meek points to an integration with Clinaris, a platform that tracks cleaning status and what type of cleaning is needed once a patient leaves a room, as an example. Integrating it with an RTLS, he says, can help hospitals turn beds faster and get the next patient in more quickly. Meek says some organizations are currently trialing the integration and evaluating the economics of it.
Additionally, integrations with medical device cybersecurity platforms are surfacing as a way to address operational gaps. Meek cites RTLS integrations with cybersecurity tools such as Censinet and Medigate. These platforms can identify vulnerabilities on networked medical devices but often lack visibility into where those devices are physically located.
In those cases, RTLS can supply the missing context. When a cybersecurity platform flags a device that needs to be patched or taken offline, RTLS can provide its location, allowing teams to quickly find the asset and address the issue. “We’re not necessarily helping with cybersecurity itself,” Meek says, “but when they do find a vulnerability on a medical device, we can then know the location of it so they can go grab it, turn it off, and patch it.”
Smarter Capital Planning
Capital planning has long been cited as a potential benefit of RTLS. But now hospitals have location data that is accurate and comprehensive enough—and integrated into the right systems—to use it as evidence in purchasing, rental, and fleet decisions.
Sonitor’s Davidson says RTLS-driven asset lifecycle management has been “a longtime promise,” but “has it been in practice? No, not really” until more mature technology and integrations converged with a stronger business need. As RTLS data is integrated with maintenance systems and ERP platforms, teams can see “what assets are truly in service, what might be sitting idle, what’s in inventory, what may be lost, and where they might be able to optimize or actually reduce their spend,” he says.
This can help avoid perceived shortages that have historically driven purchasing, he says. If clinicians can’t find IV pumps, the assumption is often that the hospital needs more—even if the existing fleet is underused or sitting idle in the wrong place.
“Teams and nurse managers can use the RTLS data to see what equipment is constantly in demand and what might be underused,” Davidson says. “That’s an insight that then allows them to not necessarily buy more equipment but have smarter distribution and placement of where equipment should be in the hospital.”
Where RTLS Is Headed
Looking ahead, RTLS vendors expect greater emphasis on predictive and data-driven operations. “Hospitals don’t just need to understand what happened yesterday; they need the ability to anticipate what’s likely to happen next,” Kontakt.io’s von Gilsa says.
At Children’s Health, senior system admin Cuong Tran describes a future where maintenance activities are driven by how equipment is actually used. “We would like to explore maintenance tasks being generated based on actual run time, movement, or zone-based rules rather than static schedules,” Tran says. “These activities would not apply to all asset models but would be an option for applying to certain cases where we could trigger on usage.”
Davidson says these types of efficiencies are becoming increasingly important as HTM departments continue to operate under staffing and budget constraints. He says that by treating location data as a foundational operational input—rather than just a way to find equipment—RTLS becomes part of a broader enterprise strategy.
“It’s not just about tracking anymore. It’s about connecting RTLS to all these disparate systems so that teams can start to run more smoothly and increasingly automate,” Davidson says. “Hospitals may not have initially expected location data to be one of their key data sources for future automation, but it absolutely is becoming that.”
ID 187455004 © Roman Samborskyi | Dreamstime.com
Alyx Arnett is editor of 24×7 Magazine. Questions or comments? Email [email protected]



