
Derrick W. VanKampen
With the increase in alarms emanating from biomedical devices in the clinical environment, and the surge in biomedical device networks and connecting systems, alarm integration rises from the nursing floor and demands our utmost attention. Nurses often complain of “alarm overload,” and, worse, nurse managers fear their staff will be infected with “alarm apathy.” What can be done to alleviate these complaints now? What can be done in the future to eradicate this apathetic virus? At Tampa General Hospital (TGH) we are trying to answer these questions and plan for an alarm environment where noise, visual alarms, and delivery to the caregiver are all taken into consideration by a collaboration of biomed, IT, and the nursing staff.
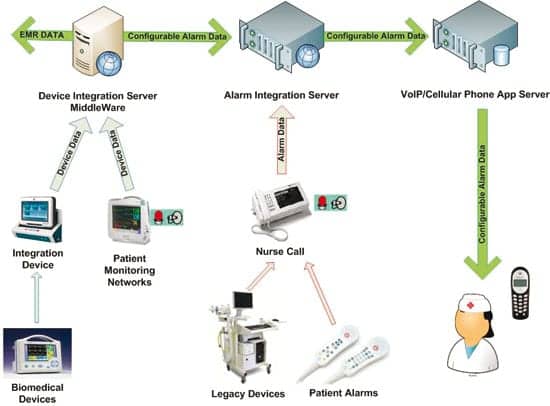
Currently at TGH, our nurse call system is connected to an Emergin alarm integration server, which directs alarms toward our Spectralink and Vocera communication devices for our clinical staff. Three different types of data feed our alarm integration server via our Rauland-Borg nurse call: standard nurse call alarms, such as staff assist, etc; biomedical device hi/lo alarms via a stereo phono jack interface into the nurse call system, such as ventilators; and standardized text messages that the clinical unit coordinator can send to various staff.
Biomed is responsible for every aspect of our nurse call system. We feel this is very appropriate based on our biomedical staff’s quick response, training, and experience in the clinical environment. Our alarm integration server is owned by IT, with access given to biomed for nurse call and communication device troubleshooting purposes. Our nursing communication devices are maintained jointly by our IT and biomed staff, with IT maintaining database aspects and biomed responding to device issues in the clinical environment.
In our current state, as we examine the causes behind “alarm overload,” the noise factor smacks us right in the face. The peeps, chirps, and gongs of various patient monitors, devices, and nurse call alarms greet you as you open the doors to our ICUs. Added to this symphony is the intermittent solo performed by the overhead paging system. The desire to increase patient and staff satisfaction by decreasing the noise level has to take into account patient safety and exist within Joint Commission standards.
In a few months we will open the first phase of a 94 private-bed NICU. This project has given us the opportunity to integrate alarms in a unique clinical environment. We will add a staff tracing system to our nurse call system and also send more data-rich biomedical alarms to our alarm integration server through our patient monitoring database server. The patient monitoring network will be “headless” and thereby voiceless, in regard to central nursing stations. In the event that our alarm integration backup server goes down, we will have individual cables with each patient monitor that can be interfaced into our nurse call, and alarms will be audibly and visually obvious. In this department we will send the alarms from our integration server to VoWi-Fi hands-free devices worn by the clinical staff. While this project will not completely resolve the noise equation, we believe it will provide a lot of information relating to biomedical alarm integration and workflow, which we can analyze, interpret, and thus form a more perfect union of alarm delivery.
At TGH we are eagerly anticipating the “go live” of our EMR next year. Biomedical device integration will play a major part in this project and will offer some interesting alarm integration possibilities. We have elected to go with a middleware company. In addition to utilizing its interface device located in the patient room, we will be using its DataCaptor server that will allow us to send one stream of biomedical device data to the EMR and another stream of filtered biomedical device alarming data to our alarm integration server, which then can filter down to the nurse communication devices.
Also eagerly anticipated is a proposed trial with a company that provides the functionality of a nursing communication device on a BlackBerry, iPhone, or iPad. It will be able to add different ring tones/vibrations for different alarms and it brings texting to the forefront, which could eliminate the need for overhead paging. If we can eliminate overhead paging in the clinical environment, we can reduce the overall noise ceiling. If, by filtering, we can separate critical alarms from noncritical alarms and direct the noncritical alarms away from an audio representation and directly to the nurse communication device, then we feel we will effectively turn down the volume of our symphony. If we can integrate all clinical alarming and send it to the same nurse communication device, then we must. If all this is done, then we will be ready to go beyond just alarm integration and into unified communications, which will provide for full functionality from a single device to include alarm integration, patient waveform viewing, vital signs validation for the EMR, biomedical device remote operation, RTLS viewing, and bar code/RFID applications, just to mention a few!
Derrick W. VanKampen, CompTIA Network+, CompTIA RFID+, certified wireless network administrator, is a biomedical device integration analyst 2 in the information technology department at Tampa General Hospital, Tampa, Fla. For more information, contact .
What’s on Your Mind?Got a gripe? A recommendation? Does someone or something deserve praise? Share your opinions and insights with your peers. Soapbox columns should be 850 to 900 words in length and can be e-mailed to . |





