A custom-built training program tackles the technician shortage with a blend of virtual learning and on-the-job training.
By Alyx Arnett
For years, clinical engineering leaders like Benjamin Duman have watched a troubling trend unfold. As experienced healthcare technology management (HTM) professionals near retirement and educational programs close their doors, the pipeline of new talent has dwindled, making it increasingly difficult to fill essential roles.
Duman, executive director of clinical engineering at Providence, a 52-hospital system spanning seven states, saw the challenge firsthand beginning around seven years ago. “I started to see a decline in the amount of candidates we had when we had job openings, let alone qualified candidates,” Duman says.
After grassroots efforts to partner with a local university to develop a pipeline proved difficult, a solution emerged from an unexpected place: a leadership conference where he heard Richard Gonzales, president of the College of Biomedical Equipment Technology (CBET), speak about the college’s work. That meeting sparked a collaboration that has resulted in a first-of-its-kind training program, tailored to Providence’s needs and designed to create a sustainable pipeline of skilled technicians.
The program combines online instruction, virtual reality (VR) labs, and on-the-job training and could offer a replicable model for health systems nationwide facing similar workforce pressures. “Our goal was to design a focused biomed program that builds and augments skillsets required for those interested in becoming an entry-level associate biomed,” says Duman.
Designing a Purpose-Built Program
Rather than adopting an off-the-shelf curriculum, Providence and CBET embarked on a six-month design process, with support from PartsSource. The goal was to build a program from the ground up that would align directly with the competencies Providence needed in its entry-level technicians. This collaborative approach was essential, Gonzales says, because one size does not fit all in modern workforce education.
“We believe that education training models need to fit our employer industry partners’ needs,” Gonzales says. “Designing a program for an industry partner as important to us as Providence, rather than saying, ‘Here’s the program, fall into this mold,’ was critical in this relationship.”
The result is an intensive hybrid program, originally 18 weeks and now expanded to 20. CBET provides the foundational online theory, supplemented by VR lab content from NVRT Labs that allows students to work on virtual medical devices. The cornerstone of the program, however, Duman says, is the on-the-job training component managed by Providence. Duman’s team provided CBET with a list of hands-on skills they wanted students to master, and the college tailored its curriculum to ensure the classroom theory prepared students for their practical work on the bench. To manage this across dozens of hospitals, the team turned to SkillNet Labs, which turned Providence’s on-the-job checklist into a mobile application.
“As new material was covered in class, techs could pull out their phone, find the related [on-the-job] items, and check them off the moment they finished,” says Mike Kritzman, founder and CEO of SkillNet Labs. “Once a task was marked complete, managers received a prompt to validate it right from their own devices. In real time, they could see who was progressing, who might need coaching, and where to focus next.”
From Facilities to the Front Lines
The program was designed to both upskill existing employees and attract new talent. The inaugural cohort of 11 students was composed entirely of Providence caregivers from diverse backgrounds, including a health coach and staff from food and nutrition services.
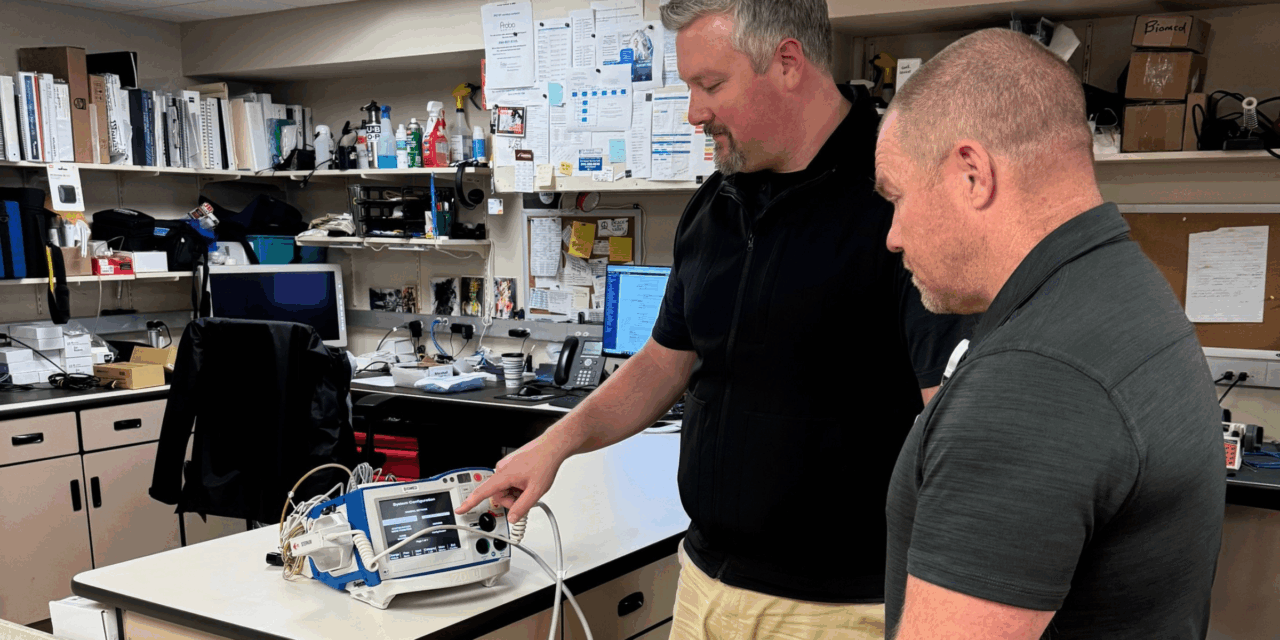
For many, it was a path to a new career within the organization they already called home. Cody Green, a technician at Providence St Patrick’s Hospital in Missoula, Mont, participated in the program after being hired into the biomed department from a facilities background three weeks before the initial cohort kicked off. “The next 18 weeks were a very valuable crash course into all aspects of biomed,” Green says.
The program gave him a fundamental understanding of the equipment, his responsibilities, and the confidence to take on more complex tasks. “Without this program, I definitely would not have the knowledge base that I have now about equipment nor the expectations of a biomed,” he says. “I was invited to work on more equipment as the team started to learn that I was going through this program.”
Providence supports employees through the program, which aligns with its tuition reimbursement benefits. A key outcome is preparing every student to take and pass the Certified Associate in Biomedical Technology (CAB-T) exam from the Association for the Advancement of Medical Instrumentation (AAMI). The program’s tuition also covers the cost of the CAB-T certification exam, removing a potential barrier for students.
For Green, the experience was so impactful that, instead of taking the CAB-T, he enrolled in Providence’s internal prep course and took the Certified Biomedical Equipment Technician exam in November. Results will be announced in January.
Investing in the Industry’s Future
The program is intended to feed into Providence’s entry-level clinical engineering openings at the local sites where participants complete their on-the-job training. Duman says retention is the goal, but placement ultimately depends on whether those sites have both the capacity to support on-the-job training and open roles to fill. The training also prepares participants for entry-level HTM roles more broadly.
“Providence is not only investing in their people and their organization, but they’re also investing in the industry,” Gonzales says. “They understand that you’re going to win some; you’re going to lose some. But it doesn’t change that necessary requirement to invest in your people and ensure quality outcomes for patients.”
With a successful start and a waiting list for future classes, the program is set to expand. For the third cohort, Duman hopes to open the program to external candidates, including friends and family of employees and local high school STEM students. This expansion is made possible by a new affiliation agreement that addresses the liability and logistical challenges of bringing non-employees into hospital environments for on-the-job training. The number of students in each cohort will be determined by the capacity of local clinical engineering departments to host them for the hands-on training.
Gonzales believes this agile, collaborative framework is the future of HTM education. “It’s shorter-term programs. It’s the ability to be agile and innovate,” he says. “Find a way around [obstacles] and find pathways and resources to support them.” It’s a model CBET is already discussing with other health systems, each with its own unique needs.
For PartsSource’s Alex Gedeon, chief operations officer and president of enterprise, the program demonstrates “what’s possible when providers, educators, and technology partners come together to strengthen the workforce and improve operational readiness.”
Photo caption: Cody Green with biomedical engineering manager Jeremy Boulter during on-the-job training
Photo credit: Providence